8 Module 8 – Nutrition and Fluid Balance
Nutrition & Fluid Balance
Learning Objectives
- Demonstrate understanding of good nutrition
- Demonstrate understanding of therapeutic diets
- Identify signs of dehydration
- Develop working knowledge of intake and output measurement
- Demonstrate understanding of alternative feeding methods
Nutrition and Diet
Resident Rights
A person’s diet is important to their overall wellbeing and physical health. It is also important for mental wellbeing and cognitive function. Because nutrient consumption is so important to a person’s health, NAs should try to make eating as enjoyable and fulfilling an experience for residents as possible. This means that personal, cultural, and social considerations are all at play.
NAs should do what they can to honor a person’s dietary preferences. Not only does this lead to better health outcomes, because people are more likely to want to eat if eating is enjoyable, but it is also an important dimension of person-centered, holistic care. Being able to make choices about what one eats is a moment of agency in circumstances that otherwise may feel disempowering.
Cultural and psychosocial needs
A person must have access to culturally relevant food. If a resident does not have culturally affirming food options available at the facility, discuss with nurses so the facility can acquire some. Culturally affirming food choices for many patients and residents are often not available, despite the fact that having such food as option leads to better health outcomes and is legally required[1].
Assist the resident in getting the facility to provide culturally appropriate meal options by requesting them from the nurse. Family members can also supply the resident with snacks and drinks that they enjoy.
Religion can also be a barrier to nutrient access in healthcare facilities. Practitioners of religions such as Judaism and Islam may uphold certain dietary restrictions, in this case Kosher and Halal respectively. Many religions involve fasting, or require vegetarianism.
If a hospital or facility does not have food that aligns with a person’s cultural and religious values, they may choose not to eat it. It is the facility and facility staff’s responsibility to create conditions in which anyone can become and remain holistically well, regardless of their cultural background.
In long-term care facilities, mealtimes can be an opportunity for residents to wear clothes they like, sit with their friends (and make new ones), socialize, and share a communal experience. It helps a resident with nutrient consumption, and positively contributes to their overall quality of life, when they enjoy and look forward to meals. NAs should make conversation with the residents during meals, facilitate introductions, and include everybody at the table in conversation.
A resident’s dietary needs will be communicated when they enter the facility, and will be included in their care plan. If you don’t see any information about cultural, religious, or personal food preferences in a resident’s plan, follow up with the nurse.
Nutrition
Nutrition is the process involved in the ingestion, digestion, absorption, and use of foods and fluids by the body. “Good nutrition” is when a person gets a sufficient amount of the right kinds of sustenance from their diet; in other words, they eat a well-balanced diet, their body can absorb what it needs to from the diet, and they consume the correct number of calories. Malnutrition occurs when a person does not absorb enough nutrients, whether because of their diet or a medical condition, and their body is weakened by insufficient sustenance.
Good nutrition is necessary for the body to function. It is also needed for new tissue growth and healing. A well-balanced diet supports immune health, mood and cognitive function, healthy elimination, a healthy circulatory system, and more. Nutrition is a consideration when providing holistic care because it is holistically important.
Insufficient nutrition can contribute to many different health problems. While good nutrition can bolster the immune system, insufficient nutrition can increase a person’s risk for infection and illness, and make any diseases they are already experiencing worse.
Whereas good nutrition allows a body to heal, insufficient nutrition can drag out a healing process or even inhibit it entirely. While good nutrition is important for cognition and awareness, malnutrition can negatively impact mental functions such as alertness, memory, orientation, decision-making, and mood regulation.
Nutrition in the geriatric population
The geriatric population will have a specific set of dietary needs and considerations.
As a person ages they lose some of their senses of taste and smell, and may find that they have difficulty swallowing due to slowed saliva production. They may also experience a lack of appetite from lowered physical activity levels.
Medications and illness may affect appetite, or the sensory experience of foods. Considering these factors emphasizes the importance of the NA’s role in making eating a positive and enjoyable experience so that residents can continue to meet their nutrient needs.
Nutrients
Nutrients are different substances within foods and beverages that a human body needs to absorb in order to function. There are six basic nutrients: water, fats, carbohydrates, proteins, vitamins, and minerals[2].
Water
Water is the most important nutrient and is essential for all bodily functions; it is an important part of our blood, keeps our cells healthy, helps our body filter out toxins, and assists in digesting food and absorbing nutrients. A person cannot live without consuming water, and would die after only a few days without it. Water is key to all bodily systems and functions.
Fats
Fats are an important part of a balanced diet, and come in four varieties. There are saturated and trans fats, of which the body requires only a very small amount, and which can increase cholesterol levels and the risk of cardiovascular disease if over-consumed. Monounsaturated fats and polyunsaturated fats, by contrast, are necessary in the diet and decrease the risk of heart disease and diabetes. Some sources of essential healthy fats are avocado, nuts and seeds, olives, and fish.
Carbohydrates
Carbs are the body’s primary source of energy, and are necessary for the body to metabolize other forms of nutrients. Carbohydrates such as whole grains and certain fruits and vegetables like corn and mango also contain fiber, which is important to healthy digestion and solid waste elimination.
Protein
Proteins are important for the body’s tissue growth and repair, and are a substantial source of energy. Proteins are also important for blood health. Good sources of protein can be found in nuts, beans, seeds, peas, some grains such as quinoa, eggs, fish, and fowl.
Vitamins
Vitamins are essential substances that perform a variety of different functions, including the health of our immune system, supporting cognitive function, bone strength, the health of our mouths and teeth, and much more.
The body cannot produce most vitamins, and many vitamins can only be properly absorbed when eaten in the right amounts and in conjunction with other vitamins and nutrients. Some vitamins are fat-soluble, which means they can be stored in the body’s fat tissue and used at a later time. Water-soluble vitamins are broken down by water and then any excess water-soluble vitamins are passed when the body eliminates.
Minerals
Minerals, like vitamins, cannot be produced by the body and must be acquired from outside sources in one’s diet. Examples of minerals are zinc, sodium, and other electrolytes necessary to balance our blood. Minerals perform a variety of different functions in the human body from fluid balance and regulating blood levels to bone strength to energy levels.
USDA MyPlate
The US Department of Agriculture (USDA) developed the “MyPlate” system to help people determine what goes into a balanced diet for their age demographic. The USDA MyPlate icon is a visual representation of what a “healthy” plate looks like, in terms of the breakdown between fruits, grains, vegetables, proteins, and dairy[3].
Some nutrition tips from myplate.gov geared towards older adult from plate are to eat a protein-rich diet to help maintain muscle mass and density, include fruits and vegetables as snacks between meals, and to eat plenty of protein and B12 fortified foods since the body’s ability to absorb this necessary vitamin lessens with age.
The USDA MyPlate system divides a “healthy” plate into five basic food groups and visually represents them so that one half of a plate is made up of fruits and vegetables, the other half is made up of grains and proteins, and dairy is represented on a small plate to the side. It is a set of recommended dietary guidelines published by the US Department of Agriculture so the public can stay up to date on changes in our scientific understanding of nutrition and health.

USDA myplate. (n.d.). Retrieved May 24, 2023, from https://www.myplate.gov/
- Fruits and vegetables are an essential food group. An abundance of leafy greens, dark green, red, and orange vegetables and fruit is especially important because of their high vitamin and mineral content. The fruit and vegetable category includes all fresh, frozen, or dehydrated fruits and vegetables, including 100 percent juice. NAs should encourage residents to eat a wide variety of fruits and vegetables every day for their beneficial nutrients and fiber.
- Grains make up a little over a quarter of the MyPlate and are foods like rice, oats, and wheat. Many foods are made using grains including pastas, cereal, bread, tortillas, and various doughs. Grains are either considered “whole” or “refined.” When a grain is refined, its outer layers are removed and only the inside of the flowering plant remains. A whole grain is one where literally the whole grain is present; its outer layers remain, which makes whole grains more nutrient dense and rich in fiber.
- Protein is slightly less than one quarter of the MyPlate. Proteins come from plant-based sources, such as legumes, soy products like tofu and tempeh, and peas. Protein is also concentrated in animal products like seafood, eggs, poultry, lean meat and red meat. If consuming animal proteins, older adults should make sure to include sea food regularly in their diet because it has fewer health detriments than red meat, and is an important source of healthy fats.
- Dairy makes up the smallest portion on the MyPlate visualization. Dairy includes any foods made from animal milk, such as yogurt and cheese. Dairy can provide important nutrients for the body, such as vitamin D and protein. Products made from soy, nuts, and oats are healthier alternatives to dairy, especially when fortified with vitamins.
Therapeutic Diets
It is the whole care team’s responsibility to make sure that the person being cared for has their nutritional needs met. This will especially involve the nursing team, doctor, dietitian, speech-language pathologist, occupational therapist, and potentially the person’s family. Sometimes a special therapeutic diet will be necessary to meet the person’s nutritional needs, or to work with a resident’s dysphagia.
Special diets are ordered for people who require a certain nutrient profile to achieve their care goals. Only a doctor can prescribe a therapeutic diet, and the special diet is then taken into account by the facility’s dietitians.
NAs must always ID residents before serving them their food, and check the resident’s ID to make sure it corresponds with the card on the meal tray. Serving somebody the incorrect food when they are on a special diet could produce serious health consequences.
Types of therapeutic diets
Doctors prescribe a wide variety of therapeutic diets. Some of these diets are intended to meet a person’s needs around food consistency and swallowing, while other diets are designed to increase or decrease the amount of particular nutrients[4]. Here are some common therapeutic diets it is useful for NAs to know about:
- Liquid diet: Only served liquid food. On a clear liquid diet the liquids are restricted to broths and juices, while on a standard liquid diet a person can have cream-based soups and ice cream.
- Soft diet: Only served foods that are soft and easily swallowed and digested.
- Pureed diet: Only served food that has been pureed into a grainy paste.
- Bland diet: No spicy or acidic foods or other foods that can irritate the digestive system.
- Lactose-free diet: Not served anything containing lactose. Lactose is a protein found in dairy products, and people who lack the ability to process this protein are considered lactose-intolerant. Some kinds of milk will still be allowed, such as lactose-free animal milk, or milk alternatives from soy, rice, oat, and nuts.
- High-fiber diet: An abundance of foods with high fiber, such as whole grains and raw fruits and vegetables. High-fiber diets can help with some digestive disorders and constipation.
- Low-fiber diet: Fiber intake is purposefully decreased by diminishing high-fiber food sources and eliminating foods with laxative properties like coffee and milk.
- Modified calorie diet: Caloric intake is raised or lowered depending on whether they need to gain weight or lose it.
- Low-sodium: Salt intake is restricted. This is an important diet for people suffering from heart or kidney disease. Sodium causes the body to retain water and places a higher workload on the human heart.
- High-protein diet: Prescribed for people who are recovering from wounds or another physical trauma. A person’s protein intake is drastically increased.
- Fluid-restricted diet: Fluid intake is restricted. Be careful not to give a person on a fluid-restricted diet fluid-based foods such as ice cream and soup.
- High-iron diet: Iron intake is increased through foods like dark leafy vegetables, legumes, and iron-enriched whole grains.
- Diabetic diet: Insulin is an enzyme that helps the body convert sugar into energy. If a person’s body does not produce enough insulin, as is the case with people with diabetes, then sugar can clog the blood and cause problems.
- A person who has diabetes must closely monitor all of their nutritional intake, and carbohydrates, fats, and proteins must all be consumed in the proper relative amounts at the right times.
- People with diabetes must avoid high-sugar foods, especially those made with processed and refined sugars.
- NAs must always serve meals exactly on time for someone on a diabetes meal plan. NAs should carefully observe the intake of a person with diabetes to see what was eaten and what was left on the tray and report this information. NAs should also report observed changes in the person’s eating habits.

- Gluten-free diet: Some people cannot process gluten (protein found in wheat and some other grains) due to celiac disease or a gluten intolerance. Gluten is common in wheat products like bread, pasta, and crackers; it can also be found in most beers, and may be used as a filler ingredient in processed foods and beauty items.
- If gluten needs to be eliminated from a person’s diet, they can turn to non-gluten alternative flours made from rice, almonds, oats, and others. The increasing recognition of celiac disease and gluten intolerance means that alternatives to gluten products have been becoming more available.
Gluten Free by Loren Klein from Noun Project (CCBY3.0)
- Vegetarian or vegan diet: A person may choose to uphold a vegetarian diet, or it may be prescribed for medical reasons. Vegetarian diets always exclude meat, though a pescatarian diet excludes all meat except seafood. A lacto-ovo vegetarian diet excludes all meat but includes milk and eggs. A lacto-vegetarian allows milk but excludes eggs, while an ovo-vegetarian excludes milk but allows eggs. A vegan diet excludes all animal products. People on vegetarian or vegan diets may need to take iron and B12 supplements.
Dysphagia
People who don’t experience difficulties swallowing may take their ability to swallow easily for granted, but those with difficulties swallowing require special care from the care team. Difficulty swallowing is called dysphagia, and people with dysphagia must be evaluated by a speech-language pathologist to determine the proper course of care[5].
Thickened liquids
People with dysphagia may be prescribed thickened liquids. This is because regular liquids, such as water and tea, can be difficult to swallow and harder to control by the mouth and throat muscles. Once a person is prescribed thickened liquids, the doctors, nurses, dietitians, and speech-language pathologist work together to determine the proper thickness to make the person’s liquids. Thickened liquids travel slowly down a person’s throat and decrease the risk of choking for people with dysphagia.
Liquids are either pre-thickened or have a thickening agent added to them. Thickened liquids will either come in a nectar consistency (a thick juice), a honey consistency (viscous like honey, pours slowly), or a pudding consistency (does not pour like a liquid – consistency of pudding). NAs must always be patient with people on thickened liquids, since getting through a thickened drink can take much more time than drinking regular water or soda.
NAs should never offer unthickened liquids, such as coffee and tea, to people prescribed thickened liquids. NAs should also remember not to leave a water pitcher in this person’s room.
Foodservice express. (2011, April 1). Dysphagia – about thickened liquids [Video]. Youtube. https://www.youtube.com/watch?v=UYBb4PrCTJk
Signs, symptoms, & strategies
Observe residents when they eat, and report any signs of difficulty swallowing to the nurse immediately. Dysphagia can be extremely dangerous if left unaddressed. If NAs notice any of the following problems while a person eats, they should report it immediately:
- Avoiding eating or eating slowly and with observable difficulty or anxiety
- Spitting food out, or small bites of food and/or pills remaining uneaten
- Saliva dribble
- Vomiting, or food/fluid exiting or entering the nostrils during consumption
- Coughing, choking, and difficulty breathing
- Eyes watering during food or fluid consumption
Difficulties swallowing puts somebody at risk for choking; they must be monitored closely during the eating process. Aspiration refers to the inhalation of food or fluids (including bodily fluids) into a person’s lungs; aspiration can cause serious problems, including choking and pneumonia, and can lead to death. To prevent choking and aspiration, NAs can deploy some of the following strategies:
- Make sure that person is in a 90 degree position sitting upright. A person is more likely to aspirate if they are reclined.
- NAs should be slow and methodical when feeding somebody, alternating between food and drink in small amounts.
- Both the NA and the person eating should focus on eating; distractions increase the likelihood of choking.
- Make sure that the person completely swallows their food before offering more. Check non-invasively – never stick fingers in the person’s mouth.
- Closely observe a person the whole time they are eating. Report signs of difficulty and discomfort immediately in case intervention is necessary.
NAs must always exercise patience, composure, and kindness when helping a person eat. If the person requires assistance and the NA is rushed the person’s emotional wellbeing be compromised and a negative association formed around mealtimes. A rushed NA is a safety hazard, because it increases the likelihood of residents choking and aspiration, and makes the NA less likely to closely observe the person as they eat.
Appetite & Comfort
A person’s appetite is distinct from their need for food. Appetite refers to a person’s desire for food and their drive to consume it, not just the need for nutrients. Many different factors can impact a person’s appetite. These are some factors that can negatively impact a person’s desire to eat:
- Weakness, illness, and confusion or disorientation
- Unpleasant odors, sights, or sounds. Making sure the person’s space is as comfortable as possible helps make eating a pleasant experience.
- Uncomfortable positioning. Make sure the person is physically comfortable and safely positioned when they eat.
- The need for oral hygiene can impact a person’s appetite. If a person finds eating difficult or unpleasant due to sensations in their mouth, NAs can report this to the nurse and alternative mouthcare strategies can be implemented.
- The need to eliminate. Always offer the bathroom before mealtime.
- Pain negatively impacts appetite.
Promoting appetite
NAs can do lots of things to promote general comfort and help make mealtimes an enjoyable experience for residents.
- Always help a resident use the bathroom before and after meals.
- Provide some oral care prior to meals by making sure that the resident’s dentures are fixed in place and free of debris.
- If a person experiences incontinence, make sure they are clean and dry before their mealtime.
- Make sure the person is positioned safely and comfortably for their meal at an upright 90-degree angle at table height. Sometimes tables or wheelchairs will need to be adjusted for a resident to eat comfortably.
- Make sure the resident has any assistive devices they need, such as hand-grips for silverware.
- Give residents as much say in their meal experience as possible. This includes their choices on what and how much to eat, and where and with whom to sit.
- Try to make eating a positive experience for residents, and always conscientiously practice patience. Remain positive and conversational throughout the meal, encourage positive socializing at the table, and assist the person as discretely as they can to ensure the resident’s dignity and sense of independence.
- Assist the resident with handwashing before and after their meal.
When assisting someone with visual impairments, describe the person’s plate of food including the type of food and its location. Always describe what is on the food tray. If the NA is feeding the person, they should describe what is on each bite. If the person is able to feed themselves, describe the food on the whole tray and describe its location using the numbers on the clock. For example, “peas at 9 o’clock, and mashed potatoes at 6 o’clock.”
Dehydration
Fluid balance
Water is essential to survival. Every single part of the human body needs water to function. Human bodies use water, and then get rid of it through sweat and elimination. An adult needs at least 1500 mL (milliliters) of water per day to survive (50 oz, or about 6 glasses of water), but should ideally have between 2000 and 2500 mL of water (about 66 – 83 oz) per day, or about 8 – 10 cups.
A person’s daily water requirement can change depending on variables like hot weather, activity levels, illness and fever, fluid loss, medications, and age.
A person’s fluids must be balanced in their body. Dehydration is when a person’s body does not have enough fluid in it. Water retention edema, by contrast, occurs when somebody has too much fluid in their body, a condition in which a person’s body retains too much water.
Water retention edema
Water retention edema can be uncomfortable; symptoms include bloating and increase of size in the abdominal area, swelling and puffiness of the arms and legs, shiny skin, heavy legs, and skin that holds a dimple after being pressed[6].
If the resident experiences shortness of breath, an irregular heartbeat, or chest pain, it could indicate fluid buildup in the lungs. Edemas can be caused by a number of factors, including being sedentary, consuming too much salt, and taking certain medications. If the NA notices any signs of edema water retention, especially stretched and shiny skin and if the skin holds a dimple after being pressed, then they should report it to the nurse immediately.
Symptoms of dehydration
If fluid output exceeds fluid intake, then dehydration occurs. Remaining properly hydrated is necessary for a person’s health, especially as they age. Peoples’ hydration needs can vary a lot depending on age and activity level, though a general guideline for daily water consumption is about 64 oz[7].
As people age they become less thirsty, but that doesn’t mean they need less water. Sometimes a doctor will prescribe “force fluids” for a resident, which just means that they should be regularly encouraged to drink. If NAs notices the resident exhibiting signs of dehydration, they should report it immediately. 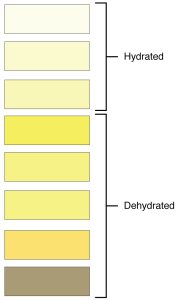
A resident may be dehydrated if:
- The resident drinks little throughout the day, and doesn’t drink at meals
- The resident has difficulty drinking from cups unassisted, experiences dysphagia, or is disoriented
- The resident frequently expresses being thirsty
- Diminished urine production
- Dry mouth and cracked lips
- Constipation
- Dark and strong-smelling urine
- Feeling weak, dizzy, disoriented, and irritable
Image by OpenStax College, CC BY 3.0
NAs are responsible for making sure residents maintain proper fluid balance. NAs should encourage residents to drink by regularly offering them fluids they like and knowing how residents like to consume fluids (ie, with or without ice, in a specific cup, etc).
Always check the care plan to see whether a person needs their liquids thickened, and always follow the posted schedule for routine fluid consumption. Ice chips and ice sticks can be offered to residents who need fluids but have a difficult time consuming them in large enough quantities in liquid form.
Fluid-restriction
Many people will require encouragement to stay adequately hydrated. However, some medical conditions will require a fluid-restricted diet, or NPO, an acronym for the Latin words for “nothing by mouth.” NPO is the most restrictive kind of fluid-restricted diets.
On a fluid restricted diet, the person will consume few if any liquids by mouth. They can drink, but only up to the point permitted by the doctor’s order.
If the person is prescribed NPO, they cannot consume any liquids and will instead receive their hydration and nutrients through their IV line. A person is put on NPO for a variety of reasons, such as preparing for or recovering from surgery, or another medical test or procedure. A person on NPO is not even permitted chewing gum.
Intake and Output (I&O) Measurement
A doctor or nurse may order that Intake and Output (I&O) measurements be kept on a patient. I&O means that the facility keeps track of all of the fluids that go into a person’s body and all of the fluids that come out. I&O records are kept to help the facility evaluate fluid balance and kidney function, to help plan medical treatment, and when the person has a special fluid order[8].
When taking intake, NAs should measure all of the fluids the person takes by mouth, as well as any fluids they take in through IV fluids and tube feedings. “Fluids” refers to all liquids, some solids like gelatin, and any food that melts at room temperature.
Output of course refers to urine, as well as vomit, diarrhea (not solid feces), and drainage from wounds. “Fluid balance” is achieved when a person’s intake and output are roughly equivalent.
Recording I&O
An I&O record is a series of tables that a facility uses to track all of a person’s fluid intake and output over 24-hour periods. All I&O measurements are taken in milliliters (mL), which is 1/1000th of a liter. One ounce is equal to thirty milliliters, or 1oz = 30 mL.
NAs must be able to perform conversations between ounces and milliliters (abbreviated as mL or cc), because some fluids may be measured in ounces. For example, if the NA serves a patient 8 ounces of water, and the patient consumed about 6 ounces, then the intake would be recorded as 180 mL (6 x 30 = 180). A helpful tip for making quick mental conversions using the multiplier 30 is to multiply the number by 3 and then add a zero to the end. In the above equation, this would look like 6 x 3 = 18, and then adding the zero so the final answer is 180.
NAs will a tool called a graduate to measure fluids. A graduate looks like a large cup with a handle and a pitcher tip, and will be marked using lines labeled with measurements in milliliters and ounces.
Calculating intake
Intake measurements are taken right after the person is served a meal, snack, or drink. Once the person is finished with their food and/or drink, take note of how much food or drink there was originally – for example, if the resident was served 4 ounces of ice cream and an 8 oz cup of tea, then 12 ounces of fluid was served.
Once the person is finished, gather whatever fluid went unconsumed, measure it, and then subtract that number from the total amount of fluid served. The total fluid minus the remaining fluid will yield the amount of fluid the person has consumed. Or, T (total) – L (leftover) = C (consumed).
So, let’s say that after 4 oz of ice cream and 8 oz of tea were served, the person has 1 oz of ice cream and 2 oz of tea leftover. First, we should put the numbers in milliliters: 1 oz x 30 = 30 mL, and 2 oz x 30 = 60 mL, and 30 + 60 = 90 mL. So 90 mL is the leftover. 12 oz x 30 = 360 mL is the total. So if T – L = the total fluids consumed, then 360 – 90 = 270 mL of fluid consumed.
To properly tally I&O at mealtimes, NAs will need to know the volumetric servings of facility dishware such as cups, bowls, dishes, pitchers, and glasses. For example, usually a cup of water is 8 oz, or 240 mL, while a bowl for cereal and milk will be about 5 oz, or 150 mL. Dish, bowl, and cup volume may vary depending on the facility.
The serving amounts will for the facility dishware will likely be listed on the I&O sheets; if they are not, always follow up with the nurse to make sure I&O records are performed correctly.
Measuring output
 To measure output, use a graduate and whatever device the person uses for urinary elimination, such as a handheld urinal, bedpan, or commode. Plastic urinals and basins for collection will likely have mL amounts marked.
To measure output, use a graduate and whatever device the person uses for urinary elimination, such as a handheld urinal, bedpan, or commode. Plastic urinals and basins for collection will likely have mL amounts marked.
After performing the opening procedure, empty the contents of the person’s voiding device into the graduate, being careful to make sure that no fluid is lost to spillage or splashing.
After carefully remembering the accurate measurement, pour the urine down the toilet, rinse the graduate and the urinal/bedpan and store them to be cleaned, and perform the closing procedure. Finally, record the output amount and the time it was taken.
I&O measurement for each patient is totaled at the end of each shift.
Image by Laboratoires Servier, CC BY-SA 3.0,
RegisteredNurseRN. (2018, February 26). Intake and Output Nursing Calculation Practice Problems NCLEX Review (CNA, LPN, RN) I and O [Video]. Youtube. https://www.youtube.com/watch?v=a6ovyZIs9tg
Assisting with feeding[9]
Persons with weakness, paralysis, casts, confusion, and other conditions may require assistance when feeding; this information will be included in their care plan and on the diet card that accompanies their meal tray.
Passing out food
When passing out food, the NA should make sure that residents who can feed themselves safely are helped first, while those who need high levels of assistance should only be given food once the NA can devote full attention to them. If a resident who requires assistance eating attempts to eat on their own, it may put them in an undignified situation or create a choking and aspiration risk.
Residents have rights around meals, such as a right to choose what they eat and drink, and a right to choose whether or not to wear a clothing protector.
Food should be served as quickly as possible so that it is appetizing for the resident. Food also must be served and eaten promptly because food that is allowed to sit at room temperature becomes a safety hazard and may induce foodborne illness. Serving food promptly helps minimize the risk of pathogens entering a person’s body through their meal.
Food safety
To keep food safe, people who handle food should wash their hands often, and keep countertops and food preparation sites as clean as possible. Different foods should stay separated to avoid cross-contamination.
Food must always be cooked thoroughly and to a safe internal temperature; if re-heating a dish, it should be re-heated to at least 165 degrees Fahrenheit. Once prepared, food should be refrigerated or frozen with two hours, or within one hour if the room is warm.
Helping someone to eat
When helping a person eat, the NA should give that person their total and full attention. Not paying full attention to a person can result in missing an important sign of difficulties eating.
It is also important from a holistic health perspective; if the NA is constantly distracted or devoting their attention elsewhere, the person needing assistance may feel like a burden, or will be less likely to ask for help when they need it.
Even if a person requires substantial assistance with eating, the NA should do everything they can to encourage the person to perform actions independently if possible, such as holding and using a napkin.
Always directly face a resident while the resident is eating. This is so the NA can pay close attention to the resident in case they have any issues chewing or swallowing, and so the resident knows they are attended to and taken care of. Face-to-face contact can put a person at ease, and make them know they are cared for; somebody who is being fed but who needs to communicate something will use their eyes and face, so it is important that the NA is paying close attention and looks directly at the resident.
Chippewa Valley Technical College. (2022, December). Preparing Clients for Meals and Assistance with Feeding. [Video]. YouTube. Video licensed under CC-BY-4.0.
Nutritional support
If a person can’t eat, or can’t eat enough, then they will require nutritional support and may need IV therapy. Enteral nutrition is the term for supplying a patient with nutrients using a tube that has been inserted into their gastro-intestinal (GI) tract. Gavage is the process that occurs when a person receives a feeding through their tube.
People using feeding tubes will be given formula; the type, amount, and scheduling will be prescribed by the doctor and included in the care plan. Enteral nutrition formula is only given at room temperature; don’t heat or chill it. The nurse will provide scheduled feedings with a syringe, or a feeding bag. If continuous feeding is ordered, the person will receive a steady supply of formula over 24 hours through the use of a feeding pump.
There are different kinds of tubing available depending on how the person needs to be fed.
- Naso-gastric (NG) tube: feeding tube is inserted through the nose, down the esophagus, and into the stomach.
- Naso-enteral tube: feeding tube is inserted through the nose and extends down into the small intestine.
- Gastrostomy tube: the doctor surgically creates an opening into the person’s stomach and inserts the feeding tube directly into the person’s stomach. A gastrostomy is a surgical opening that leads into a person’s stomach.
- Jejunostomy tube: the feeding tube is inserted into a jejunostomy, or a surgical opening at the upper portion of the small intestine.
In Illinois, NAs will never insert feeding tubes, clean feeding tubes, or provide feedings through feeding tubes. They will likely assist the nurse with performing some of these actions though. Always closely follow instructions when assisting the nurse.
NAs will need to be conscious of the tubing when they provide care. Make sure that the area around the tubing is cleaned frequently, and apply lubricant to keep the area free from chapping and dryness. NAs should make sure the tubing is smooth, free of kinks and wrinkles, and securely in place. Always check in to make sure that the person is comfortable and calm.
Complications
Report to the nurse if anything seems wrong with the person or the person’s tubing, such as the tubing having come undone, respiratory difficulty, aspiration, signs of infection at the tube site, or any sources of irritation or discomfort for the person.
Report any irregularities and signs of unwanted side affects immediately. Symptoms of enteral nutrition complications include:
- nausea
- discomfort
- vomiting
- abdominal swelling
- coughing
- complaints of indigestion or heartburn
- fever
- respiratory distress
- increased pulse
- complaints of flatulence
- diarrhea
Nasal feeding tubes can irritate and create pressure on the nose, alter the shape of a person’s nostrils, and create pressure ulcers. NAs should report any irregularities to the nurse as soon as possible.
Aspiration is a major risk when a person is being fed through a tube. Aspiration can occur during the tube insertion, if the tube is moved out of place, or if formula is regurgitated.
NAs can help prevent aspiration by placing the person in Fowler’s or semi-Fowler’s position before they are fed, and maintaining Fowler’s or semi-Fowler’s for a while post-feeding. Always follow the care plan and nurse’s directions when assisting a person who uses feeding tubes.
Parenteral nutrition
Parenteral nutrition is similar to enteral nutrition, except rather than a feeding tube that leads to the person’s GI tract, nutrients will be provided for the person through a catheter inserted directly into a vein. In this case, nutrients never pass through the person’s GI tract at all and instead the nutrient solution is given directly into the person’s bloodstream. This is also called “total parenteral nutrition” or “TPN.” TPN is used when the person cannot receive oral or enteral feedings.
NAs are never responsible for TPN care or performing any of the functions of TPN. The NA’s role with persons who need TPN is to assist with basic needs and ADLs, and to carefully observe the person for any adverse responses to their TPN.
Report any adverse responses to TPN promptly, including:
- fever and chills
- signs of infection
- chest pain
- difficulty breathing
- nausea and vomiting
- diarrhea
- thirst
- irregular heartbeat
- weakness
- sweating
- paleness
- trembling
- disorientation or behavior changes
Patients using an arterial catheter or an IV line are at increased risk for infection, so any signs and symptoms of infection must be responded to quickly.
IV Therapy
IV therapy is the administration of fluids directly into a person’s bloodstream. IV therapy may be ordered for a person when they are unable to drink regularly, for people who need to rapidly replenish vitamins and minerals, to provide sugars, or to give a person blood or drugs.
NAs are not responsible for IV therapy, and should always closely follow the nurse’s instructions when caring for somebody receiving IV therapy.
Intra-venous lines are either peripheral or central. A peripheral IV is located away from the center of the body, such as in a person’s hand or calf. A central IV is located close to the person’s heart.
A central venous line is a kind of catheter than is inserted into a persons chest or upper respiratory area to make IV lines more convenient. They are used when somebody needs IV therapy for a long period of time or frequent blood drawings. Central venous sites are used for parenteral nutrition, providing large amounts of fluid, long-term and repeated IV therapy, and to administer some drugs.

NAs must maintain rigorous safety standards when caring for people receiving IV therapy. NAs should never change the position of the IV clamps or adjust any controls on the IV pumps. If they accidentally bump the machine or nudge the IV out of place, they should record the incident and tell the nurse immediately.
- Tell the RN immediately if no fluid is dripping from a person’s IV line, or if the rate of fluid is too fast or too slow. There will be a “time tape” on the IV bag to display how much fluid should be given over a period of time. If the fluid does not match the time tape, tell the nurse at once.
- NAs will never be responsible for starting or maintaining IV therapy, regulating the IV flow rate, changing the IV bag, or giving blood or drugs through an IV line. Your responsibility will be to clean the area around the IV site and to make the person as comfortable as possible.
- Always ask for help or clarification if you are unsure about how to perform a delegated task, or whether the task falls within your scope of practice.
Key Takeaways
- Good nutrition is key to holistic health. Malnutrition negatively impacts every system in the body, including mental and psycho-social wellbeing. Good nutrition involves absorbing adequate amounts of essential nutrients like water, proteins, fats, vitamins, and minerals.
- Therapeutic diets may be necessary for residents with specific dietary needs or preferences, dysphagia, diabetes, or other conditions. Always check the care plan to see whether a special diet is ordered; when a resident needs a special diet, be especially careful that they only receive food that accords with their diet.
- Our bodies need water to function; dehydration can be an extremely dangerous condition. As a person ages their sense of thirst diminishes, but their need for water does not, which leaves them prone to dehydration. If residents display signs of dehydration, report it to the nurse immediately.
- NAs will need to keep track of fluid intake and output (I&O) for some residents. I&O measurement involves tracking all of the fluids that somebody consumes orally or by IV and tube feeding, and all of the fluids that they release through urinating, vomiting, and diarrhea.
- Residents may require the use of alternative feeding methods when they cannot consume any or enough nutrients using conventional means. Some often used alternative feeding methods include enteral and parenteral nutrition. Enteral nutrition is supplying someone with nutrients through tubing that leads into their gastrointestinal tract. Parenteral nutrition involves supplying someone with nutrients through a direct line into their bloodstream, bypassing the GI tract entirely.
Comprehension Questions
1) If a facility does not have food that meets someone’s culturally relevant preferences or religious diet, the facility should …
a. Ask the resident’s family to supply their meals
b. Suggest that the resident alters their diet so they can remain nourished in their new circumstances
c. Adhere to the resident’s right by procuring culturally or religiously appropriate food
d. Do nothing
2) Malnutrition refers to … (Select the best answer)
a. Consistently eating fewer calories than recommended
b. Absorbing less nutrients is than necessary to remain healthy
c. Drinking too little water and eating too few vitamins and minerals
d. Eating too many unhealthy foods
3) Respond to the following sentences with T (true) or F (false).
____ The six basic nutrients are water, fats, carbohydrates, protein, vitamins, and minerals.
____ A healthy, balanced diet contains more protein than carbohydrates.
____ Fruits, vegetables, and whole grains are good sources of fiber.
____ A human body’s ability to absorb nutrients increases with age.
____ Fortified dairy alternatives from soy, oats, and nuts are healthy alternatives to dairy.
4) What are some signs and symptoms of dysphagia? Select all that apply.
a. Excessive hunger and eagerness to eat
b. Coughing or choking during food or fluid consumption
c. Saliva dribble
d. Pausing in between bits of food
e. Anxiety around or during meal times
5) When providing nutrition assistance to someone with visual impairments, NAs should … ?
a. Vividly describe the color of the food
b. Say “here comes some good food” when feeding the resident an especially delicious bite
c. Describe the location of the food on the plate using the face of a clock, and describe the food in an appetizing way
d. Check the resident’s ID at least three times
6) If a resident receives 12 oz of fluid from an IV bag, drinks a 10 oz milkshake, and drinks 2 cups of green tea, what is their total fluid intake in mL?
a. 1,130
b. 1,170
c. 1,140
d. 1,200
7) If a resident drinks one cup of water, eats a grilled cheese sandwich with one cup of liquidy tomato soup, and finishes it off with ½ cup of ice cream, what is their meal’s total fluid intake in cc’s?
a. 1,000
b. 930
c. 960
d. 900
8) If a resident receives 900 mL of fluid from an IV bag, leaves two ounces of juice in a regular sized cup after drinking the rest, and then drinks a 10 oz mug of hot cocoa, what was their total fluid intake in mL for the afternoon?
a. 1,400
b. 1,380
c. 1,320
d. 1,290
9) If a resident eats a 4 oz cup of jello and one cup of ice chips, leaves 3 oz in a cup of coffee, receives 10 oz of fluid from an IV, and voids 200 mL of urine, what is their fluid intake in mL?
a. 610
b. 600
c. 810
d. 840
10) Respond to the following sentences with T (true) or F (false).
____ NAs may be responsible for inserting cleaning feeding tubes if the task is properly delegated.
____ Residents only have a limited time window where the NA will be able to assist them with their meal, so they should eat quickly to accommodate the staff’s schedule.
____ Residents receiving naso-gastric enteral nutrition will require especially attentive skin care around their nose.
____ “TPN” stands for Total Parenteral Nosh.
____ NAs will never be responsible for beginning or adjusting IV therapy.
11) Nutrition and fluid balance deals closely with the Big Three, especially concerning matters of Resident Rights and Safety. What is at least one example of an important Resident Rights consideration when facilitating a resident’s nutrition? What is at least one example of a safety consideration when facilitating a resident’s nutrition and fluid balance? As a nursing assistant, how would you handle each consideration listed?
12) You are assisting a resident with their meal in a common area. The resident likes to eat in their geri-chair; today they are experiencing a lot of back pain, and ask if they could please recline to a 60-degree angle to eat their meal. How would you respond to the resident and why?
- Raj, M. (2021, October 7). What's on the menu matters in healthcare for diverse patients. The Conversation. https://theconversation.com/whats-on-the-menu-matters-in-health-care-for-diverse-patients-166931 ↵
- Dugan, D. (2020). Nursing assisting: A foundation in caregiving (5th ed.), Chapter 14. Hartman. ↵
- The USDA also published a set of recommendations specifically geared towards older adults: https://www.myplate.gov/life-stages/older-adults ↵
- Sorrentino, S. A., & Remmert, L. N. (2019). Mosby's essentials for nursing assistants (6th ed.), Chapter 23. Elsevier. ↵
- Speyer, R., Cordier, R., Farneti, D., Nascimento, W., Pilz, W., Verin, E., Walshe, M., & Woisard, V. (2022). White Paper by the European Society for Swallowing Disorders: Screening and Non-instrumental Assessment for Dysphagia in Adults. Dysphagia, 37(2), 333–349. https://doi.org/10.1007/s00455-021-10283-7 ↵
- Staff, M. C. (2023, January 4). Edema. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/edema/symptoms-causes/syc-20366493 ↵
- Paulis, S. J. C., Everink, I. H. J., Halfens, R. J. G., Lohrmann, C., & Schols, J. M. G. A. (2022). Dehydration in the nursing home: Recognition and interventions taken by Dutch nursing staff. Journal of advanced nursing, 78(4), 1044–1054. https://doi.org/10.1111/jan.15032 ↵
- Sorrentino, S. A., & Remmert, L. N. (2019). Mosby's essentials for nursing assistants (6th ed.). Elsevier. ↵
- Nursing Assistant by Chippewa Valley Technical College, Chapters 5 and 6 is licensed under a Creative Commons Attribution 4.0 International License, except where otherwise noted. ↵
The process of consuming food, breaking it down, and converting it to energy
A deficit in necessary nutrients
Diabetes is a disease that prevents the body from using insulin to regulate blood sugar and other nutrient absorption
Difficulty swallowing
Inhaling solid or liquid matter
Desire for food and motivation to eat
A lack of adequate fluids in the body
"Nothing by Mouth." Acronym used for patients who cannot consume anything by mouth, and will receive all of their hydration and nutrients via IV therapy.
Intake and Output measurements are ordered when a facility wants to keep track of the amount of everything that goes into and comes out of a resident's body.
The fluids that go into someone's body
The fluids that exit a person's body, except for sweat
When bits of one food dish get into another. This is a problem when residents have specific food needs and diets.
Supplying nutrients through a tube inserted at a place along the gastro-intestinal tract
The process of supplying enteral nutrition
Nutrients provided by IV therapy
Ordered when a person can only receive nutrients through parenteral nutrition, and never by mouth or tube feeding.
Directly administering fluids into someone's blood stream
A longer-term catheter placed for more convenient IV therapy
The set of actions that a particular nurse or nursing worker can perform given their legally defined role, their agency and facility job description, and their training.
