4 Module 4 – Infection Prevention
Infection Prevention
Learning Objectives
- Differentiate between medical & surgical asepsis
- Demonstrate proper handwashing technique
- Develop understanding of Standard Precautions, Bloodborne Pathogen Standard, & types of Isolation
- Demonstrate understanding of Chain of Infection
What is an infection?
An infection is a disease that results from the invasion and growth of microbes in the body. It is a major safety and health hazard, and if unnoticed or left untreated can result in serious complications or death.
Infection control refers to the set of practices and procedures that individuals and facilities use to protect patients, residents, visitors, and staff from infection. Infection control is exceptionally important, and should be something that NAs always have at the forefront of their minds.
Microorganisms are extremely small beings such as bacteria and viruses. Microorganisms are everywhere; they are on every surface we touch, in the air we breathe, in various sources of water, and in our bodies. Microorganisms tend to prefer areas that are dark and damp.
A person’s microbiome is the ecosystem of bacteria that help us live. Human beings need our microbiome bacteria for gut health and other beneficial functions. Some people take pro-biotic medicine or foods to foster their microbiome.
Microorganisms that cause harm to people are called pathogens.
When pathogens, or dangerous microbes, are consistently exposed to anti-infection measures, they can adapt and become resistant. Antibiotic resistant bacteria are a serious problem in healthcare facilities.
TED Ed. (2014, August 7). What causes antibiotic resistance? – Kevin Wu [Video]. Youtube. https://www.youtube.com/watch?v=znnp-Ivj2ek
Infection control terminology
Infection control terminology usually fall under three general categories: words describing the body’s defense system, words describing microorganisms and infections, and words discussing asepsis[1].
Words describing the body’s defense system:
- Antigens are foreign substances that initiate an immune response in the body. Antigens include pathogens, toxins, and any foreign substance that can be harmful to one’s body and ought to activate an immune response.
- Antibodies are proteins deployed by the body’s immune system that bind to and destroy antigens.
- Normal flora is a term for the normal microbes that live in certain areas of a healthy human body. For instance, the discussion above about the human microbiome is in reference to our normal flora.
Words describing microorganisms and infections:
- An object or space is contaminated when it contains potentially harmful microbes; contamination is the opposite of asepsis. Not all microorganisms are harmful; in fact, some are essential to human health. Non-harmful microorganisms are nonpathogenic.
- Contaminated surfaces should be cleaned and disinfected. One cleans a surface by applying products and friction to reduce the presence of microbes. Disinfecting a surface involves destroying the bacteria with chemicals like bleach, alcohol, and peroxide.
- An infection is an invasion of human tissue by pathogenic microbes. Most pathogens are combatable with disinfection techniques.
Sterilization techniques will be necessary to adequately combat spores and other hearty microbes that aren’t killed using standard disinfection.
- Pathogens will have varying degrees of virulence; virulence is a pathogen’s relative ability to cause disease.
Words describing techniques to combat infection:
- Sterilization refers to practices that destroy all microorganisms on a given surface using high temperatures, auto-clave pressure, and steam. “Sterile” is a difficult standard to reach. NAs will not be able to work in a completely sterile environment, but they should make sure that surfaces and hands are disinfected.
- Asepsis is the process of keeping surfaces and hands free of microorganisms. Aseptic practices are essential to safety and infection control. Part of maintaining asepsis is always applying Standard Precautions in the workplace.
- Standard Precautions assumes that all bodily fluids are contaminated. Anytime an NA comes into contact with a bodily fluid, they should automatically treat it as if they know for a fact that it contains dangerous pathogens. An example of a Standard Precaution is to always wear gloves when providing hands-on care, even if the person does not appear to be sick. This ensures that potential infection risks are immediately treated with a high degree of caution, and routinizes practices meant to minimize the spread of pathogens.
Communicable diseases
A communicable disease is a disease that can be spread from one person to another. Spread occurs through direct contact with the person, such as by being in physical contact or by breathing the same air as they do. Spread can also occur through indirect contact, such as by touching objects recently handled by the infected person[2].
A contagious disease is a communicable disease that spreads easily and quickly. Non-communicable diseases are diseases that can’t spread from person to person, such as diabetes.
A body has a natural set of defense mechanisms to prevent and combat infections. The body’s skin, mucous membranes that protect our eyes, nose, and ears, and other defense mechanisms are in place to stop, trap, or remove pathogens to keep them from entering the body, or to kill them quickly once they do. Tools like fevers, the deployment of white blood cells, and other immune responses are to fight the infection once the pathogen has started reproducing within the person’s body.
If someone has a bacterial infection, they may be prescribed anti-biotics. Anti-biotics target some microorganisms. However, if anti-biotics are ineffective, it is likely that the person is suffering a viral infection, for which antibiotics won’t be an effective treatment.
Asepsis
NAs can work to minimize the spread of communicable diseases by practicing good asepsis technique. NAs should utilize medical asepsis techniques to minimize the risk of spreading infections from person to person, or from one part of a person’s body to another part of their body. It also works to reduce the risk of reinfection, which occurs when one person becomes infected multiple times with the same pathogen[3].
Medical asepsis refers to the set of techniques healthcare staff use to keep a facility as clean and sanitized as possible. Techniques like regular handwashing, disinfecting surfaces, and wearing personal protective equipment (PPE) are all part of medical asepsis.
Medical asepsis cannot make an environment totally free of potential pathogens, let alone microorganisms. To make an object or area completely free of microorganisms involves sterilization, or the getting rid of all microorganisms, which is a technique used as part of surgical asepsis.
Surgical asepsis is different from medical asepsis in that it gets rid of all microorganisms, while medical asepsis gets rid of most microorganisms. Surgical asepsis is difficult to maintain, and requires that specific steps be taken. Sometimes procedures requiring sterile technique will require that NAs receive special training before they are allowed to assist.
Handwashing
Handwashing is essential to good asepsis technique. It is the most important thing you can do to practice infection control Washing one’s hands is something most people do regularly, but it is important to know how to do it well. Good handwashing will involve:
- Make sure to remove rings and jewelry prior to washing one’s hands to ensure a thorough clean. Items like rings and watches may also harbor bacteria and can be disinfected with hot soapy water.
- Rinse one’s hands under warm running water.
- Use antimicrobial soap and scrub one’s hands, including one’s fingernails and any other surface area where bacteria could accumulate. Scrubbing should last for at least 30 seconds – 1 minute.
- Rinse one’s hands under warm running water, and dry them.
Video by Allie Tiller is licensed under CC BY-NC 4.0
Infection control is part of the Big Three

Infection Control is the third pillar of the Big Three, in addition to Residents’ Rights and Safety, because NAs should always keep it in mind while they are working. It closely relates to the other two pillars of the Big Three.
Residents have a right to a comfortable and safe environment, so they also have a right to be free of infection to the extent that it is possible, and to have their infections promptly noticed and treated should they occur. Similarly, a resident who is regularly at a high-risk for potentially dangerous infections cannot be considered safe. Infection control is an essential aspect of providing effective care.

Noticing and treating infections
Noticing, treating, and minimizing the further spread of infections are parts of infection control. How can NAs observe and notice infections?
Inflammation occurs when tissue swells, and becomes discolored. Inflammation can occur because of damage to tissue, or as an immune response[4].
There are many symptoms of inflammation beyond observable redness and swelling, such as:
- Mild fevers
- Pain, tenderness, and limited use in the impacted part of the body
- Nausea
- General aches and discomfort
The above symptoms may indicate an immune response to the presence of infection.
The presence of infection symptoms
Everybody responds to pathogens differently, and the symptoms of a person’s infection and infection response can vary depending on multiple factors.
The virulence of microbes can vary. Virulence is a word that refers to how harmful different pathogens are. The more virulent and highly concentrated a pathogen is, the more likely it is to produce a harmful infection.
The overall health of the person and the general condition of their immune system impacts their susceptibility to infection. Proper nutrition and hydration are necessary for maintaining a robust immune system. Age, genes, and comorbidities are also relevant factors.
Emotional stress and emotional or physical exhaustion can have significant impacts on the immune system. It is important that residents do things that they enjoy, and find engaging and relaxing. This has a real impact on the immune system’s ability to fight off infections.
Symptoms of infection
The signs and symptoms of infection vary widely. They include:
- fever
- chills
- increased pulse and respiratory rate
- pain and tenderness
- fatigue
- loss of appetite
- nausea
- vomiting
- diarrhea
- joint pain
- confusion
- rashes
- sores on mucous membranes
- redness or swelling
- discharge from an infected area
- heat or warmth emanating from a body part
- the limited use of a body part
- headaches
Report any of these symptoms to the nurse and record them in the chart.
Some different kinds of infection
A localized infection is an infection that impacts a specific area, such as an infected wound. Localized infections can sometimes spread to other parts of the body. Microorganisms that are normal flora in one area of the body may be pathogenic in another.
A generalized infection is an infection that broadly affects a specific area, such as pneumonia, a rash all over the body, pink eye in both eyes, or an infection in the brain.
A systemic infection is an infection that has entered the blood stream and is therefore being carried throughout the body system; septicemia, or sepsis, is an example of this type of infection.
Healthcare-Acquired Infections (HAIs)
Healthcare-acquired infections (HAIs) are infections that develop while a person is being cared for in a healthcare facility or home-care setting. HAIs are common and dangerous, with roughly 1.7 millions and infections and 99,000 associated deaths each year.
32% of HAIs are urinary tract infections (UTIs). Residents or patients that use urinary catheters are at heightened risk for UTIs. NAs can help minimize the risk of UTIs by not leaving urinary catheters in place for extended periods of time, and by keeping the catheter and surrounding area clean. Catheter-associated urinary tract infections have the acronym CAUTI.
22% of HAIs are surgical site infections. NAs can help minimize surgical site infections by observing the site closely and closely following medical sepsis when caring for the site as it heals[5]. Other HAIS include developing pneumonia by using a ventilator, and some blood infections that result from surgeries or medical equipment.
The CDC now estimates that as many of one-third of US hospitals fail to follow the CDC’s guidelines for handwashing and other basic infection control measures, even though universal strict adherence to clean-hand policies could prevent roughly 20,000 HAI attributed deaths each year[6].
Healthcare facilities should be a place of care and healing, and it is devastating and ironic when the care someone receives results in the infection that kills them.
Multi-drug resistant organisms (MDROs)
Some HAIs are caused by multidrug-resistant organisms (MDROs), which are microbes capable of resisting the effects of antibiotics. This occurs when an organism is capable of adapting quickly in response to antibiotic treatment; rather than the antibiotic getting rid of the organism, the organism adapts so the antibiotic is no longer effective.
MDROs are rampant in healthcare facilities, and pose serious health risks to patients and residents. Three MDROs NAs should be familiar with are MRSA, c. diff., and VRE[7].
MRSA
MRSA, pronounced mer-za, is an acronym for methicillin-resistant Staphylococcus aureus.
MRSA is capable of withstanding the effects of the powerful antibiotic methicillin.
- MRSA usually manifests as a skin infection, but can also infect surgical wounds, the bloodstream, lungs, or urinary tract. It is usually either a generalized or systemic infection.
- MRSA is spread by direct contact; since the bacteria lives on our skin, touch tends to be the medium of contagion. People can contract MRSA through skin to skin contact with an infected person or by touching a contaminated object.
- MRSA changes and mutates all the time to remain resistant to antibiotics. The people most susceptible to severe MRSA are the elderly, people with weakened or compromised immune systems, and people who use tubing and implanted devices. Tubing and implants increase risk of severe MRSA because they give the bacteria a clear portal of entry into the bloodstream.
- Treatment and guidelines: A person with MRSA will be treated with an antibiotic therapy. When caring for a person with MRSA, NAs should make sure to keep any drainage from the infection contained and not let it spread to other areas of the skin or to surfaces or objects in the room.
- Exceptional hand hygiene is required, including the use of gloves when touching a patient or contaminated surfaces, and a gown when there is potential for any contamination of one’s clothing. A person infected with MRSA should not share any of their items with anyone.
C. diff
Clostridium difficile, or diff for short, is a bacterial pathogen that can develop when someone is taking anti-biotics. C.diff is a naturally occurring gut bacteria that is usually kept in balance by other bacteria in the gut microbiome. When someone takes an antibiotic that throws the gut biome out of balance, concentrations of c.diff can reach dangerous levels and cause serious illness.
According to the CDC, likelihood of reinfection with c.diff is high, and one in eleven people over the age of sixty-five who contract c.diff will die within one month[8].
C.diff is contagious. Wash your hands often, shower after your shift every day, and do not use a shared restroom while experiencing diarrhea. C.diff spores can lie dormant on a surface for five months and are not killed by alcohol hand sanitizers. Soap and water are the best defense against c.diff.
Symptoms of c.diff include:
- frequent diarrhea
- fever
- stomach pain
- loss of appetite
- nausea
If these symptoms are observed in a patient or in oneself, alert a nurse immediately.
Treatment for c.diff may include a fecal microbiota transplant (FMT). A FMT involves transplanting stool from a healthy individual into the colon of the person with the infection. This counteracts the c.diff by reintroducing necessary normal flora back into the colon.
VRE
VRE is the acronym for Vancomycin resistant Enterococcus. Enterococcus is a species of bacteria that are part of the intestinal tract’s normal flora. VRE can enter the bloodstream and cause meningitis, pneumonia, or an infection in the heart.
The symptoms of VRE manifest differently depending on the location of the infection. General symptoms of VRE include:
- drainage from a would
- fever
- chills
- fatigue
- redness and swelling
VRE is spread via direct contact between people or between a person and a contaminated object. NAs can help prevent the spread of VRE by practicing meticulous hand hygiene and disinfecting surfaces with a bleach solution. NAs should wear protective items like gloves and gowns whenever they are at risk of contamination.
The Chain of Infection
The Chain of Infection is a way of thinking about how disease spreads from one person to the next. It is a sequential loop that starts with a harmful bacteria and ends with a person’s infection; the cycle the starts again, since the infection will allow the pathogen to proliferate and spread.
The chain of infection progresses: 1. Causative agent > 2. Reservoir > 3. Portal of exit > 4. Mode of transmission > 5. Portal of Entry > 6. Susceptible host
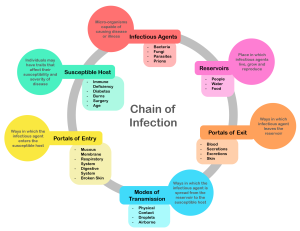
Image by Genieieiop, CC BY-SA 4.0,
- Causative agent: the pathogenic microbe that infects a person and causes illness. Causative agents could be bacteria, fungi, or viruses.
- Reservoir: surface or host where causative agent lives. The reservoir for a pathogenic microbe could be the surface of a piece of equipment or furniture, or in the food, water, and air. Animals and humans can also be reservoirs for pathogens. Microbes tend to prefer warm and oxygen-rich environments, and tend to grow better at body temperature. Many are capable of surviving on hard surfaces and in linen. Treat contaminated surfaces and linen with care.
- Portal of exit: the pathogen’s means of exiting the reservoir. In the case of human or animal reservoirs, portals of exit can include things like mucus, waste, spit, breath, and blood. A portal of entry is a pathogen’s means of entering a new host.
- Mode of transmission: the means the microbe uses to travel from a reservoir to a host, or from one host to another host. Different pathogens travel via different modes of transmission; some require contact, while others may be airborne or travel through the different medium of respiratory droplets.
- Vector transmission of a pathogen occurs when an infectious agent transfers a pathogen to another host, while vehicle transmission occurs when a pathogen enters a host from a substance or surface.
- Host: a hospitable environment for a pathogen to reproduce in, and a launchpad from which it can travel and infect other hosts. A human body can spread pathogens more efficiently than pathogens can spread themselves by interacting dynamically with their environment (breathing, coughing, touching things).
- People who are immune-compromised, elderly, or experiencing a health condition (whether chronic or acute) are at increased risk of becoming a host to an infection.
- People who live in nursing homes are at an increased risk of infection because of the higher amount of pathogenic microbes contained in the facility; because of the high concentration of people and microbes in such facilities residents are more likely to come into contact with pathogens, and are less likely to be able to successfully defend themselves against the infection.
Try out this interactive infection control game: https://www.wisc-online.com/learn/career-clusters/health-science/nur1603/chain-of-infection
Breaking the chain
There are many different things healthcare staff can do to “break the chain” of infection. When we break the chain, it means we take steps to interrupt the spread of pathogens; if one link in the chain is broken, it can prevent someone from contracting (and then spreading) what might otherwise be a harmful infection.
Here are some basic precautions that facilities and facility staff should implement:
- Wash hands before and after every care task
- Use personal protective equipment (PPE)
- Deploy isolation techniques when a person develops an infection
- Identify the infection and the type of microbe that causes it
- Facility staff should keep themselves generally healthy; overall health in the form of nutrition, hydration, sleep, and exercise is important for maintaining a robust immune system.
- Cleaning and disinfecting all equipment
- Always use aseptic technique
- Make sure residences have good airflow
- Keep hands moisturized so they do not crack and create a portal of entry
Standard Precautions
The Center for Disease Control (CDC) is an organization in the federal government that performs a variety of public health functions. The CDC researches and publishes information on diseases and issues guidelines on how the public should respond to disease. The CDC has an infection-prevention system used in healthcare facilities meant to minimize the risk of infections spreading[9].
The CDC has guidelines on the kinds of precautionary measures that must be taken to prevent infection. The two levels of precautions are Standard Precautions and Transmission-based Precautions.
Standard Precautions are a set of precautions that healthcare staff use all of the time, with all of their patients or residents. The basic idea behind Standard Precautions is to always treat blood and other bodily fluids, nonintact skin, and mucus membranes (eyes, nostrils, mouth, sex organs, and rectum) as though one is certain they are infected.
Gloves: Standard Precautions require the use of gloves whenever there is the possibility of coming into contact with bodily fluids, nonintact skin or other tissues, and mucus membranes.
- Always wash your hands immediately before and after putting on gloves; only use a pair of gloves for the procedure, and then quickly remove them.
- Do not touch dirty objects with clean gloves, or clean objects with dirty gloves.
- Wear gloves whenever using objects like razor blades, needles, or anything else that might cause a person to bleed.
PPE: Other personal protective equipment (PPE) such as gowns, face shields, face masks, protective goggles may be required in addition to gloves if staff members may get bodily fluids on their clothes or face while administering care.

Image by National Institutes of Health (NIH) is licensed under CC BY-NC 2.0.
Bloodborne Pathogen Standard: An important aspect of Standard Precautions is to also follow OSHA’s Bloodborne Pathogen Standard. As part of the Bloodborne Pathogen Standard, employers are required to keep labeled “Hazard” bins for needles and sharps, as well as to provide employees with training and information on how to avoid an accidental needle stick, and other aspects of keeping oneself safe from bloodborne infections like HIV and Hepatitis B and C. As part of OSHA’s legBloodborne Pathogen Standardislation, employers must teach employees how to handle bloodborne pathogen exposure, maintain an exposure control plan, universally implement Standard Precautions, and utilize PPE.
- Biohazards: A biohazard is any substance or object that carries a risk of infection, especially infection with a bloodborne illness. NAs must always put needles and other sharps into the labeled biohazard bin. Biohazardous non-sharp objects, such as a bloody or soiled piece of linen, will also have specific containers. NAs should always follow their facility policies on waste disposal, and should dispose of hazardous waste, or potentially contaminated objects, quickly in accordance with facility policies.
- If an employee has an exposure to blood or another bodily fluid, also called an exposure incident, they will have to fill out an exposure report form and follow up on any necessary medical tests.
Montana State Fund. (2020, March 2). Health care bloodborne pathogen safety [Video]. Youtube. https://www.youtube.com/watch?v=j2favjW1GqQ
Transmission-Based Precautions
Transmission-Based Precautions are deployed when a patient or resident is sick or has had an exposure and is suspected to become sick. They are precautions meant to prevent the transmission of illness once it is present and use isolation and heightened anti-infection techniques to limit is spread.
Transmission-Based Precautions require the use of specific pieces of PPE depending on the kind of pathogen or illness the person is exhibiting. Nurses will tell the NA what kind of PPE each person’s transmission precautions require; some facilities have signs on patients’ doors that describe the transmission precaution and PPE required.
All Transmission-Based Precautions also include Standard Precautions and washing one’s hands before entering and after leaving the room.
The three different kinds of Transmission-Based Precautions are airborne, droplet, and contact precautions.
- Airborne: Airborne Precautions are put in place for people who may spread pathogens that are expelled into the air and may remain there long enough to be inhaled by or land on a new person. Airborne infection isolation rooms (AIIR) are necessary for people under airborne precautions; AIIRs have increased air circulation and filtration to dispose of infected air quickly and to make sure no other parts of the facility are infected. Staff must wear a N95 respirator mask, and keep the door and windows closed at all times.
- Droplet: Droplet precautions are applied for people with pathogens that transmit through droplets of moisture that are expelled and either remain in the air or settle on surfaces. Droplet precautions require a respiratory mask be worn in the room at all times. Droplet precautions may require a restriction on visitors.
- Contact: Contact precautions are used when a person has an infection that is spread by direct or indirect contact. Contact precautions require the use of gloves and a gown. People requiring contact precautions cannot share equipment or linens with others; if two people must share a piece of equipment then it needs to be thoroughly disinfected between each use.
Isolation
All transmission-based precautions include isolating the person. If a person needs to be isolated due to transmission-based precautions, NAs should be aware of the negative impact that isolation can have on a person’s wellbeing, especially when it comes to their psychosocial needs. The experience can be taxing on a person.
Isolation makes somebody more vulnerable to infringements on their rights as patients and residents. NAs should always recognize that residents in isolation are at greater risk of having their rights infringed upon; when someone requires isolation, never let their call light go unattended and make sure to check in on them frequently to provide care and moments of human interaction.
Fronheiser, A. (2017, June 15). Transmission based precautions [Video]. Youtube. https://www.youtube.com/watch?v=qL-Eyq62-zc
PPE
The CDC and OSHA recommend the use of personal protective equipment (PPE) for Standard Precautions, the Bloodborne Pathogen Standard, and for Transmission-Based Precautions. PPE is used to protect care team members from acquiring any of the communicable diseases that they work hard to treat. Some different kinds of PPE are gloves, gowns, goggles and face shields, and masks and respirators.
If a patient requires a specific piece of PPE the nurse will usually say something, but it is important for NAs to be able to identify risk levels themselves and be able to apply the appropriate response. Different conditions will require different pieces of PPE – for instance, a person with pneumonia will require different kinds of PPE than a person with chicken pox.
Different isolation precautions will require different kinds of PPE. Discuss such precautions with the nurse, and when in doubt always ask. PPE protects both its wearer and every person they interact with afterwards; if you think it might be necessary, then it is. Employers are obligated to provide staff with PPE.
What PPE would you need when: transporting someone in a wheelchair? Responding to an emergency involving spurting blood? Cleaning a patient who had experienced diarrhea? Taking someone’s vital signs? Providing perineal care, or care of the genital and anal region? While emptying a catheter drainage bag? Consider the kinds of risk these activities put someone in, and the PPE someone could use to protect themselves. Write for 5 minutes, and discuss your response with a friend or classmate.
Donning and Doffing: When donning, or putting on, a full set of PPE, one should go in the order of gown, then the mask/respirator, then the goggles or face shield, and finally the gloves. When doffing, or removing, PPE one should go in the order of gloves, then goggles/face shield, then gown, and mask last.
Registered Nurse RN. (2020, May 29). PPE training video: Donning and doffing PPE nursing skill [Video]. Youtube. https://www.youtube.com/watch?v=iwvnA_b9Q8Y
Disposing of waste
Healthcare teams use many objects that, after their use, need to be disposed of. Always practice Standard Precautions while handling contaminated material. However, some material is considered more contaminated or more dangerous than others.
Healthcare facilities use a two-bag system for disposing of waste. Biohazardous waste is disposed of in “red bags,” bright orange trash bags labeled as containing biohazards. Non-biohazardous waste is disposed of in clear waste bags.
Image by stonebird is licensed under CC BY-NC-SA 2.0.
Non-biohazardous waste is still considered contaminated or “dirty.” The items that can be disposed of in clear waste bags (non-biohazardous) include household waste such as food and food containers, paper products, non-bloody PPE, and IV bags.
Bio-hazardous materials require a bit more of a multi-step process to be properly disposed of. Because even the outside of the bag of biohazards is considered contaminated, biohazardous materials need to be double-bagged.
The double-bagging process involves one person who bags the material inside the room and one who stands outside with a red bag, or a labeled biohazard bag, folded over their hands. The bag from inside the room is placed inside the red bag, and is then transferred to the dirty utility room or the hazardous waste container.
Key Takeaways
- Infection control is part of the Big Three. NAs should think critically about applying infection control measures in everything they do.
- Medical asepsis is used all the time, and refers to techniques like regular handwashing and disinfecting surfaces and equipment. Surgical asepsis is used to remove all microorganisms from a surface; surgical asepsis often deploys sterile technique, for which NAs will need special training to perform.
- The Chain of Infection refers to the cycle of pathogens from living on a surface or in a host, to entering a new host, to creating an infection and spreading through the host’s activities. Healthcare staff are responsible for breaking the chain of infection.
- Standard Precautions and the Bloodborne Pathogen Standard should be applied all the time; the gist of these frameworks involves considering any and all bodily fluids as contaminated, and protecting yourself accordingly. During transmission-based precautions, a resident may be placed in either airborne, droplet, or contact isolation; different kinds of isolation require different kinds of PPE, though they all require heightened caution. Isolation is hard on a person; watch out for the negative psychosocial impacts of isolation precautions.
Comprehension Questions
1) What sort of environment is best for pathogens to live and reproduce in?
a. An icy area
b. A cup full of bleach
c. A damp and dark area
d. A hot, dry, and sunny area
2) Respond to the following sentences with T (true) or F (false).
____ Pathogens are microbes that can cause infection.
____ Antibodies are foreign substances that activate an immune response.
____ A person’s gut biome is one example of their normal flora.
____ If a resident’s napkin falls off their meal tray and onto the floor, it is contaminated.
____ Medical asepsis requires sterile technique.
3) Medical asepsis includes which of the following? Select all that apply.
a. Regular handwashing
b. Isolation
d. Standard Precautions
e. The Bloodborne Pathogen Standard
4) Which of the following are symptoms of an infection?
a. Inflammation and redness in an area
b. Bruising
c. Mild fever
d. Confusion
e. Changes in personality
f. Headaches
g. Dry skin
5) Respond to the following sentences with T (true) or F (false).
____ A systemic infection only impacts a specific area of the body.
____ An infected wound is an example of a localized infection.
____ Healthcare-acquired infections (HAIs) are serious problems in medical facilities.
____ Normal flora are never harmful to human bodies.
____ MDROs are pathogens that develop resistance to drugs and become even more dangerous.
6) Which of the following PPE is required for Droplet Precautions?
a. Frequent hand hygiene
b. An Airborne Infection Isolation Room
c. A mask or respirator
d. A gown
7) Please put the links of the Chain of Infection in order.
8) Why is it important for NAs to spend extra time with people in isolation rooms due to infection precautions?
a. Because the more time exposed patients spend with healthy staff, the less likely they are to become sick.
b. NAs need practice being around sick people.
c. Isolation makes it difficult for someone to meet their psychosocial needs; NAs can offer some human connection when visitors are otherwise restricted.
e. NAs should spend time around sick people to build up their own immune system.
9) What are some techniques NAs can use to break the Chain of Infection? Select all that apply.
a. Keep themselves in good health so they have a robust immune system.
b. Use regular hand hygiene.
c. Treat sick patients kindly so they are motivated to get better.
d. Closely observe residents and patients for signs of illness and infection so they can be caught early.
e. Covering your mouth when you cough.
10) Respond to the following sentences with T (true) or F (false).
____ MRSA requires airborne transmission precautions.
____ VRE is sometimes treated using a fecal microbiota transplant.
____ C. diff is an MDRO that is usually part of the human gut biome’s normal flora.
____ Only nurses and doctors are responsible for breaking the Chain of Infection, because it requires specific training.
____ Standard Precautions are practiced as a way to make breaking the Chain of Infection a habit for all healthcare staff.
11) Imagine that you see a fellow NA administer a routine injection for a resident. You notice that they do not use gloves to administer the injection, and then set the needle on a countertop while performing some more care tasks. What safety precaution does this violate? How would you perform this care task differently?
12) Why is Infection Control included as part of the Big Three? What do Infection Control measures have to do with Resident Rights and Safety? Try to come up with at least two connections for both Resident Rights and Safety.
- Glossary; Infection prevention terms. (2011). https://www.vdh.virginia.gov/content/uploads/sites/13/2016/03/Glossary.pdf ↵
- Staff Writer. (2023, February 5). Standard Precautions, Transmission Based, Surgical Asepsis: NCLEX-RN. RegisteredNursing.org. https://www.registerednursing.org/nclex/standard-precautions-transmission-based-surgical-asepsis/ ↵
- Staff Writer. (2023, February 5). Standard Precautions, Transmission Based, Surgical Asepsis: NCLEX-RN. RegisteredNursing.org. https://www.registerednursing.org/nclex/standard-precautions-transmission-based-surgical-asepsis/ ↵
- Sorrentino, S. A., & Remmert, L. N. (2019). Mosby's essentials for nursing assistants (6th ed.), Chapter 13. Elsevier. ↵
- Healthcare-Acquired infections. (n.d.). Patient Care Link. Retrieved April 27, 2023, from https://www.patientcarelink.org/improving-patient-care/healthcare-acquired-infections-hais/ ↵
- CDC. (2021). Infrastructure and routine practices. https://www.cdc.gov/infectioncontrol/guidelines/healthcare-personnel/infrastructure.html ↵
- Dugan, D. (2020). Nursing assisting: A foundation in caregiving (5th ed.), Chapter 6. Hartman. ↵
- CDC. (2021). C. diff (Clostridioides difficile). https://www.cdc.gov/cdiff/index.html ↵
- Staff Writer. (2023, February 5). Standard Precautions, Transmission Based, Surgical Asepsis: NCLEX-RN. RegisteredNursing.org. https://www.registerednursing.org/nclex/standard-precautions-transmission-based-surgical-asepsis/ ↵
Disease resulting from the presence of harmful microbes
Part of the Big Three. Infection control refers to practices that prevent harmful microbes from spreading. Infection control practices include hand hygiene, wearing PPE, isolation, and sanitizing contaminated objects.
Small, living creatures like germs and viruses
The ecosystem of microorganisms that make their home in the human body
Harmful microorganisms
Foreign substance that stimulates an immune response
Proteins that bind to antigens in the blood and destroy them
Microbes that are usually found in a particular area of the body. Normal flora is unharmful, but may become harmful if it travels to areas of the body it is not supposed to be in.
A term designating when a surface may contain pathogens. A surface is contaminated when the presence of pathogens is possible.
Minimizing or removing the presence of microbes
Destroying all or close to all bacteria on a surface using a chemical cleanser
How effective a pathogen is at causing disease
Destroying all microbes on a surface
Minimum standard of caution when interacting with a person's body fluids. It assumes that all bodily fluids carry an infectious pathogen and treats them as such.
A disease that can spread
Communicable disease that spreads quickly
Asepsis techniques used in all circumstances
Equipment such as masks, gowns, and gloves meant to protect healthcare staff from contracting or spreading infection
The set of aseptic practices used for removing all microorganisms from an area or surface
Procedures used to execute surgical asepsis and remove all microorganisms from a surface or an object
The swelling and discoloration of tissue
Infection that only impacts a specific area of the body
An infection that broadly impacts a specific body area or system, such as a rash all over one's skin or pneumonia.
An infection that is in the blood stream and impact all bodily systems
Infections that develop while a person is receiving medical care, often as a result of the care itself.
Organisms that adapt to protect themselves from the use of multiple different kinds of antibiotics
Pathogenic microbe that evokes an immune response
Where pathogenic microbes live in between hosts
A pathogen's way of exiting the reservoir
How the pathogen travels
A hospitable environment for a pathogen to reproduce in, and infect others from.
A federal organization that passes research, guidelines, and regulations on public health and disease prevention.
Occupational Safety and Health Administration, a federal regulative body that works to ensure safe working conditions
A set of standards used to protect employees from contracting a bloodborne illness
Specific precautions to use when a patient is suspected or known to carry and contagious disease
