13 Module 13 – End of Life Care
End of Life Care
Learning Objectives
- Apply knowledge of the impact of pain on quality of life
- Demonstrate understanding of the need for sleep
- Develop understanding of the need for end-of-life care
- Demonstrate understanding of the stages of grief
People need care at the end of their life, often in the form of palliative care. Palliative care means care that is given to make a person as comfortable as possible as they live with an illness that will be the cause of their death. Hospice care is ordered when the person’s prognosis is less than six months. NAs who are assisting with end-of-life care should always use a compassionate, holistic, person-centered approach that keeps in mind the goal of comfort, rather than cure[1].
Pain and Comfort
A person receiving palliative care or hospice care will likely experience pain and discomfort as part of their illness process. All the time, but particularly in the final stages of their life, residents have a right to comfort, rest, and sleep. Comfort, rest, and sleep are essential for a person’s overall wellbeing. Disruptions in a person’s comfort, rest, and sleep have a negative impact on a person’s holistic wellbeing (physical, emotional, spiritual).
A person is only comfortable when they are free from pain, anxiety, and emotional distress. A person is only comfortable if they are relaxed and at ease. NAs should always as a person what the NA can do to make them more comfortable. Rather than asking a yes-or-no question, asking “is there anything I can do to make you more comfortable” may allow a person more freedom to respond.
Pain looks different for everybody. NAs must never assume that somebody is free from pain, unless that person explicitly tells you they are free from pain. Sometimes a person in pain may need to be prompted more than once before they admit to being uncomfortable; NAs should get to know a person so they develop a sense of when the person is uncomfortable, and can ask follow-up questions when discussing their comfort.
GeriCare. (2021, March 2). What is pain? [Video]. Youtube. https://www.youtube.com/watch?v=att6sLZmKdU
Pain is a warning from the body that signals that some kind of damage is present. Though not technically a vital sign, it is sometimes considered the “fifth vital sign” because it provides caregivers with important information that may require a nursing response.
If a person says they are in pain, they are in pain. NAs must never second-guess a person’s testimony of pain. Refusing to believe somebody who says that they are in pain is an abusive behavior, and is not acceptable within a person-centered care framework.
The experience of pain
Pain is a subjective experience, which means that everybody experiences and relates to pain differently. Some people may be comfortable expressing their pain and distress to others, while others may not want to express their pain and would rather grit their teeth through it. NAs should be attentive to a person’s pain signals when they are not comfortable expressing their pain openly.
- A person’s past experiences with pain, the idea of pain, and the idea of “resilience” or “weakness” can make a person less inclined to express their pain.
- Anxiety may prevent a person from expressing their pain if the person is not usually comfortable asking for help, or who believe that by voicing pain they are a burden on someone. NAs should go out of their way to assure anxious residents that they are there to help, that they are happy to provide care, and that NAs always prefer when a person in pain directly expresses that pain to them.
- Rest and sleep and pain are in a cyclical relationship. If a person is not rested and cannot sleep properly then they are more likely to experience pain, well, painfully. If a person experiences heightened pain levels, then they are less likely to rejuvenate through sleep and rest.
- One’s personal, familial, and cultural background plays a part in how they relate to pain. If somebody comes from a culture that discourages expressing one’s pain, or if they have internalized the belief that pain is something that ought to be suffered through rather than alleviated, they may be less likely to be honest about their pain levels with the care team.
Types of pain
Pain is felt differently by everyone, but there are different kinds of general pain that people can use to communicate the character and quality of their pain.
- Acute pain is sudden onset pain due to tissue damage resulting from injury, disease, trauma, or surgery. Acute pain lasts less than 6 months and diminishes as the damaged tissue heals.
- Chronic pain is pain that lasts longer than 6 months and persists after any tissue damage has healed. Chronic illnesses such as arthritis may be at the root of chronic pain.
- Radiating pain is pain felt in one part of the body that is caused by a problem in another part of the body. Examples may be developing a headache because of a toothache, or pain in the left arm and jaw during a heart attack.
When asking about pain, NAs can use a 1 – 10 scale to ask the person to rate their pain, in addition to asking questions about how the pain feels; is it a burning sensation, a stabbing sensation, does it feel like a shock? etcetera. Always follow facility protocol and the care plan when it comes to how to ask patients about their pain levels and quality.
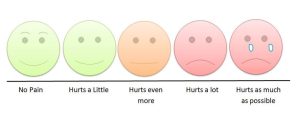
Image by Robert Weis, CC BY-SA 4.0
Reporting and recording pain
NAs must carefully report and record when residents relay information about their pain. When recording communications about pain, NAs should write down the exact words that the person uses to describe their pain. The specific language the person uses can give nurses and doctors important clues into the pain’s underlying cause[2].
These are some basic pieces of information NAs should make sure to record:
- Location of the pain (placement in the body)
- When the pain began, how long it lasted or is lasting
- The intensity of the pain over time, including any changes in the intensity of the pain throughout its duration
- Any other descriptive features the person can offer, including any observations they have about positions, activities, or conditions that alleviate the pain or make it worse.
Assessing pain in non-verbal residents
Sometimes a person will not be able to communicate their pain levels, or will display pain signals without admitting to being in pain. If a person is unable to or won’t communicate their pain, NAs will need to observe them for other signs and symptoms of pain. If a resident displays or expresses any of the following symptoms of pain, NAs should report it to the nurse promptly and record it in the person’s chart[3].
- Changes in appetite
- Dizziness, lightheadedness, and vertigo
- Nausea and/or vomiting
- Numbness and/or tingling
- Increases in pulse, respirations, and blood pressure
- Pale skin
- Difficulty sleeping
- Sweating
- Crying and/or gasping, grunting, and sighing
- Tightening of the facial muscles, including squeezing the eyes closed, grinding teeth, clenching the jaw, grimacing or frowning
- Changes in behavior such as increased restlessness, agitation, or distraction
NAs and pain management
So what is the NA’s role with regard to pain management during end-of-life care? NAs should focus on providing excellent basic care and making the person as comfortable as possible, including by being a calming and positive presence for them during moments of pain.
- Regular repositioning is an important aspect of pain management. Always follow the care plan and respond promptly to the resident’s preferences.
- Keep the person’s bed linens neat and wrinkle free. This goes hand in hand with repositioning as a strategy to prevent pressure injuries and ulcers. The last thing somebody needs during end-of-life care is to develop yet another source of physical discomfort.
- Assist with the person’s elimination needs promptly. Pain increases a person’s chance of incontinence, and having an unmet need to eliminate adds yet another source of discomfort.
- Apply cold and heat therapies as directed by the nurse, doctor, and by the care plan.
NAs can be a comforting presence to a person in pain by telling stories, conversing, and providing distraction and relaxation through guided imagery techniques. Recorded guided meditations or calming video and music compilations can also help relax a person. Ask a person what their favorite movie or music is, and see if you can play it as a pleasant means of distraction. The most important thing is to be attentive, responsive, and do one’s best to anticipate ways the person can be distracted from their discomfort.
Other factors impacting comfort
Comfort is different for everybody, and different people will all feel most comfortable in slightly different conditions. NAs should be aware of some factors that relate to comfort so they can best meet the person’s comfort preferences. Some factors that affect comfort are:
- Activity level – immobility comes with serious complication; if it is in the person’s care plan, NAs should encourage activity and exercise. Regular activity promotes physical comfort and high-quality rest.
- Room temperature – older adults are more susceptible to cold. OBRA requires that nursing home facilities be kept between 71- and 81-degrees Fahrenheit. If a person still experiences chill at 81 degrees, NAs can offer blankets.
- Ventilation and airflow – rooms with stale and stuffy air are unpleasant to be in. NAs can improve the airflow in a room by opening the person’s door, or opening a window depending on the outdoor air quality.
- Noise level – some people are bother by noise and prefer quiet. NAs can close the person’s door, and request that anybody having audible conversations in the hallway move to a common area instead. If the person would prefer noise to silence, NAs can play some of the resident’s favorite music.
- Odors – odors can be unpleasant and induce discomfort. NAs can reduce odors by providing attentive perineal, skin, and bathing care. NAs should not smoke on the job, but if they must they should make sure to thoroughly wash their hands, and be conscious of odors’ tendency to stick to clothing. Breath odors can be controlled by regular teeth brushing, mints, and gum.
- Lighting – lighting should be comfortable and safe. If a person finds harsh overhead lighting uncomfortable, NAs can see about options for softer and ambient lighting. If the person has difficulty seeing, adequate lighting will be an important safety consideration.
Sleep and Rest
Sleep is a basic need; without sleep, a person cannot function physically, cognitively, emotionally, or socially. Sleep is a state of unconsciousness that allows the mind and body to rest, restore its energy, and process information from the day. During sleep voluntary muscle activity is reduced and the metabolism is lowered. All of the person’s vital signs are lower than when the person is awake.
Sleep allows for restoration and healing. Adequate sleep promotes physical healing and tissue repair. It also helps a person to lower their stress levels and anxiety, and gain emotional clarity.
The Economist. (2019, January 30). What happens when we sleep? [Video]. Youtube. https://www.youtube.com/watch?v=eTgNgGO_bLs
Sleep can sometimes be elusive, or difficult to achieve, especially when somebody is in a new and unfamiliar environment; their regular routines and rhythms will be disrupted and thrown out of balance, which may result in poor and dysregulated sleep[4].
- Make sure that all rooms have sufficient pillows and blankets.
- Make oneself available for conversation as the resident goes to sleep; trying to sleep in an unfamiliar environment can be difficult, and some people may appreciate a friendly presence.
- Make sure the lighting, noise, ventilation, and odor needs are met. Try to maintain quiet when a resident is sleeping, whether at night or as an afternoon nap.
- Remember that people who are ill will need more sleep than usual.
- A person’s nutrition and exercise can impact their sleep. If a resident is having difficulty sleeping and consumes caffeine regularly throughout the day, NAs can recommend that they lower or eliminate caffeine intake. Regular activity and exercise increases tiredness and can make it easier for a person to fall asleep.
Mental health problems such as anxiety and depression can negatively impact a person’s sleep. If a resident reports feelings of anxiety and depression, tell a nurse so they can develop strategies to address the resident’s mental wellbeing. Mental health professionals are available for persons with ongoing mental health concerns.
Sleep disorders
Sleep disorders can influence a person’s ability to sleep. Sleep disorders can be caused by a variety of factors including illnesses (physical and mental), medication, problems with the environment such as noise and lighting, and embodied distractions such as pain or the need to urinate[5]. 
Insomnia is a chronic condition where the person cannot fall asleep or cannot stay asleep through the night. Some people may require medication to manage their insomnia, while others may be able to mitigate it through lifestyle changes.
Image by Videoplasty.com, CC BY-SA 4.0
Sleep deprivation is a condition where the amount or quality of sleep is seriously decreased. Many different factors can cause sleep deprivation; the best way to address sleep deprivation is to diagnose the underlying cause and work from there. Minimizing caffeine and increasing activity levels is often a first step.
Sleepwalking occurs when a person remains asleep but gets up and performs activities that they normally would only perform while awake. The sleepwalker is usually unaware and will have no memory of the event. If NAs encounter somebody sleepwalking they should gently guide them back to bed. People can become startled when woken from a sleepwalking episode; NAs should always interact gently with a person sleepwalking.
Caring for residents with disordered sleep
NAs can care for people in ways that allow them to get as much rest as they can.
- Care should be planned for uninterrupted rest; do not waken somebody to provide care unless it is necessary.
- Flexible bed times and waking times allow residents to be on their own schedule and sleep in the way best suited to their body’s rhythm.
- A warm bath or shower before going to bed can relax a person and soothe their muscles. A backrub can also help a person physically relax.
- Follow regular bedtime routines, offer the use of the bathroom, and make sure residents with incontinence are clean and dry.
- Provide a comfortable temperature, in addition to cozy and loose-fitting pajamas, and plenty of soft linens.
- Make sure the person feels safe. Sometimes this is accomplished by creating a pleasant sleeping environment, other times a person may need some conversation, music, or a guided meditation to mentally prepare for sleep.
- Pay attention to the resident’s routines, body language, and stated preferences. NAs should ask residents what makes them most comfortable, and remember their answer.
End-of-Life Care
Terminal illness
A terminal illness is a disease or injury for which there is no reasonable expectation of recovery[6]. Many illnesses and diseases have no cure, and are known to eventually be the cause of death. Similarly, after some injuries the body is not able to function, and recovery is not expected. Examples include serious damage to the brain and internal organs. When a disease or injury is reasonably expected to end in death, it is deemed terminal.
Doctors cannot truly predict when a terminal illness will end a person’s life. They may be able to make educated guesses, but so many different and sometimes inexplicable factors go into how a person responds to terminal illness that a precise prediction is ultimately impossible. 
The care outcome for a person with a terminal illness will be strongly influenced by a person’s will to live and their experience of hope. A person with a terminal illness will likely prolong their life by engaging in activities they enjoy, remaining active in their community and social circle, and bringing an awareness of the value of their life into their daily reality.
ElouiseFord, CC BY-SA 4.0 At the same time, the nursing staff should be realistic about the person’s impending death. Language should not be softened because of a desire to make things easier on a person, since this can have the opposite impact; shying away from the terms “death” and “dying” is infantilizing and may prevent the person from reckoning with their circumstance.
Everybody dies. Death is a reality that brings meaning to the living of a life. Rather than ruminating on the fear and anxiety of death, NAs should consider how they can talk about death in a way that treats it as a natural, necessary stage of the life process.
Attitudes towards death
People have many different attitudes about death. Some of these attitudes are personal, while others relate to someone’s cultural and religious background. Some people believe in a paradise-like afterlife, others believe in reincarnation, and other believe that nothing much happens at all. Death rites, prayer and scripture readings, and funeral services are common in various religious and cultural practices.
NAs should ask if the person they are caring for would be comfortable sharing some of their attitudes and beliefs about death, and simply listen to them. It may give someone comfort to remind themselves of a framework for understanding their own death in the greater scheme of things[7].
Many people strengthen their religious convictions, or seek out new ones, when they are made aware of the immanence of their death. This sort of spiritual grasping may be based on a genuine sense of spiritual awakening, a response to fear and anxiety, or both.
Adults may fear or resent their death. They may fear experiencing pain and suffering upon death, dying fearful and alone, and having their privacy and dignity invaded as they are dying. They may fear being separated from their loved ones, or leaving their dependents and community without them. Perhaps they were not ready to die, and still had plans, hopes, dreams or ambitions. These are difficult things to make peace with; if a person is able to use their spirituality and religion to make peace with the fact of their death, this should be encouraged.
Religious attitudes towards death
A person’s religious beliefs and cultural background will impact how they relate to their death, and the approaches to care that will be most helpful with the person’s spiritual outlook in mind. Someone who believes that their soul is headed for an eternity of either paradise or torture may be comforted by the idea leaving the earthly plane, or concerned and anxious for the fate of their soul. A person’s spiritual ideas about death may be a source of comfort, a source of anxiety, or both as they are dying.
Someone who believes in an afterlife with Heaven and Hell will likely want different spiritual care and communication than somebody who believes in reincarnation. When someone is reincarnated their essence or their constitutive elements returns to the total cycle of life and they are reborn, either as a human, animal, a celestial entity, or something else. They may want to reflect on their life and the aspects of it to which they assign high spiritual importance to consider their cyclical journey towards Nirvana.
In all cases, NAs will listen to residents’ thoughts and feelings about their death, and tell the nurse if they request any spiritual or religious services. All residents have a right to meeting their spiritual needs.
Meeting a person’s spiritual needs as they are dying is associated with better psychological and physiological outcomes. In other words, by fully meeting a terminally ill person’s spiritual needs, the healthcare team can help them live longer and ease the discomfort and emotional turmoil of their passing[8].
Spiritual Needs
A dying person has psychological, social, and spiritual needs. NAs will have to address the full scope of a person’s needs in order to relieve their suffering as they are dying. A steady listening ear and comforting touch can be important to someone who feels scared and alone in these moments. Some people may request to see a spiritual leader or take part in religious practices; NAs should tell a nurse immediately if a person wants to see a religious official or to have religious rites performed.
- A dying person’s religious objects may become especially important to them as the they are dying. NAs must handle such objects with respect, and encourage the resident to find comfort in their religious practices if it is appropriate.
- NAs should provide a person with privacy when they want to pray or meditate, unless the person requests that they remain.
- A dying person may feel the need to take a confessional approach with whoever will listen. NAs must never judge anybody for the things they are told; a dying person deserves peace and dignity, even if they want to confess sources of guilt and other things they want to get off of their chest before passing. This information must be kept private and may only be shared with the person’s nurse. NAs should avoid discussing their own spiritual and religious beliefs with the dying person.
- NAs should spend quality time with dying residents. They may be tempted to avoid dying people, especially if they are uncomfortable with death themselves. A dying person deserves opportunities for human connection, and may carry anxiety about the possibility of dying alone.
- Never respond to a resident’s fear of death with clichés or personal stock-phrases. It is always best to acknowledge a resident’s fear and anxiety and attentively listen, and then inform the nurse. The person may benefit from the skilled care of a mental health professional or social worker.
Providing End-of-Life Care
End-of-life care is the care and support given to somebody and their family during the time surrounding their death. End-of-life care may range anywhere from a single day to multiple months. A person’s death may come on suddenly, or be a gradual and drawn-out process. Healthcare teams see and interact with death regularly – a person’s attitudes, feelings, and associations with death will impact the end-of-life care they provide.
Most people die either in a hospital or a long-term care facility, and hospice care is becoming a more widely used option[9]. A person in hospice care will likely be aware that they are dying. Such awareness means that they will have a unique set of psychological and spiritual needs. The healthcare team should provide every service available to make the person as holistically comfortable and secure as possible.
In order to provide good care to someone who is dying, NAs will need to bring an awareness of the dying process into their communications to approach the person with caring, kindness, and respect. They will also need to bring an understanding of their own feelings about death and dying into their care to remain positive, un-phased, and authentic in their interactions with the dying person.
A person’s emotional and spiritual experiences and beliefs regarding death can increase their suffering[10]. Perhaps they feel that they are leaving things unattended to, or have not gathered closure on important questions; the experience of dying can be disempowering and leave someone feeling out of control.
Being able to participate in the decision-making process about one’s own end-of-life care can help make someone feel more agential in their dying process. It also gives them an opportunity to prepare themselves for death. If somebody is unable to make their own decisions about end-of-life care, it may prevent them from reckoning frankly and honestly with their own death. Reckoning honestly with death is an important part of maintaining relationships and finding a sense of closure.
TEDx Talks. (2018, August 14). Making end of life care matter | Deb Wilkes | TEDxSouthampton [Video]. Youtube. https://www.youtube.com/watch?v=Lr6gvVnuW-0
Palliative and Hospice care
One decision that persons with a terminal illness will face is whether to enter palliative care or hospice care[11].
Hospice care is one form of palliative care, though palliative care is broader than hospice care. The goal of palliative care is symptom and pain management; while palliative care is given to people who have a terminal illness, it does not necessarily mean that somebody’s death is immanent. Someone with congestive heart failure may live decades after diagnosis with the right kind of palliative care. Palliative care uses a person-centered approach to keep someone’s holistic quality of life as high as possible while living with an incurable condition.
GeriCare. (2021, February). What you need to know about palliative care [Video]. Youtube. https://www.youtube.com/watch?v=KZ9ZXS4C3No
Supporting the person’s family is an important dimension of palliative care. Palliative care encourages residents to continue doing the things they enjoy, seeing the people they love, and generally leading a full life. Palliative care emphasizes symptom management, emotional wellbeing, and spiritual services and care.
Hospice care is palliative in the sense that it aims to make a person as comfortable and pain-free as possible; the goal is to facilitate a dignified death. Hospice also provides services to the person’s family and the healthcare team after the person’s death in the form of emotional care and support groups. Hospice care may be provided in a nursing facility or as home healthcare.
Stages of Grief
In her book On Death and Dying (1969), Dr. Elisabeth Kübler-Ross came up with the Five Stages of Grief model[12]. She breaks down the grief process of a dying person, or somebody coping the dying of a loved one, into five general stages: Denial, Anger, Bargaining, Depression, and Acceptance.
A dying person may not move through these stages linearly, they may not even start with denial. A person can also occupy more than one stage at a time, or shift back and forth between different stages depending on the day. It is not guaranteed that each dying person will experience all five stages. The stages apply both to the person who is dying, and to others in their life who have to reckon with the impending death of a loved one.
- Stage 1, Denial: The person experiences a refusal to recognize that they are dying. Denial can manifest in a refusal to make arrangements for one’s death, an insistence that the tests gave a false result, or an unwillingness to discuss one’s feelings about their health and death.
- Stage 2, Anger: Once somebody recognizes that they are dying, they may respond to this realization with anger ang rage. Their anger may be directed at their family, friends, the healthcare team, god, themselves, or at everything at once. NAs should always meet the anger of a dying person with compassion and empathy, and remember not to take their anger personally. Becoming angry is a normal part of reckoning with one’s death.
- Stage 3, Bargaining: After admitting to themselves that they really are dying, the person may try to strike a deal with the universe, god or God, or some other higher power. Such bargaining usually involves a promise to live differently in exchange for elongated life, perhaps to see their children grow up or another event after which the person believes they will have achieved some closure.
- Stage 4, Depression: Depression is a condition where a person becomes too sad and mournful to function normally. Perhaps they question the meaningfulness of their remaining time, withdraw from the people around them, and cannot bring themselves to perform simple tasks or care for their own wellbeing. The care team must be kind, patient, and understanding with people who are experiencing this kind of depression.
- Stage 5, Acceptance: Some people will come to accept their own death before it happens. This allows them to make final arrangements and say goodbye. People at this stage may seem detached from the world, or they may seem extra present. However a person responds to accepting their death, the care team should be available to listen, talk with, and assist the person with anything they’d like to do before dying.
These stages are descriptive, rather than prescriptive. In other words, nobody should try to move a dying person through the stages of grief. Instead, the stages provide a framework for thinking about and interpreting how somebody is responding to their death. The care team’s role is to listen and make the person as comfortable as possible, without trying to get the person to think or feel in a different way.
LevelUpRN. (2021, July 28). Stages and Types of Grief, Types of Comfort Care – Fundamentals of Nursing [Video]. Youtube. https://www.youtube.com/watch?v=9nRHY3oIIeU
Comfort
A central goal of caring for a dying person is to keep them physically comfortable. Residents have a Right to attentive and compassionate care at the time surrounding their death. As a person is dying all of their bodily systems will begin to slow down; their vitals will lower, they may lose control over their stomach and elimination, and they may become confused, disoriented, or appear vacant. They may become unable to express discomfort or ask for their needs to be met. NAs should remain attentive to the person’s needs even as they move closer toward death. Residents have a right to comfort and attentive care[13].
- Frequent oral hygiene

- Carefully clean the person’s nose so it is free from crusts and drainage
- Regular skin care, bathing, and repositioning to promote cleanliness and prevent pressure ulcers
- Changing the bed linens and the resident’s clothing as needed
- Careful perineal care, especially after elimination
- Good body alignment in bed to promote comfort and easy rest
- Attentive pain management. NAs should report to the nurse if the resident appears to be in pain or discomfort.
A dying person may have personal objects with them, such as sentimental mementos, pictures of their family and friends, flowers, or religious objects. Such items should be positioned where the resident can always see them; carefully hand the objects to the person if they seem like they want to hold or touch them, and put them back when the person is finished.
Approaching death
A person’s comfort needs will change as they approach the moment of their death. Their bodily systems will lose function, and they may become uncomfortable as their body loses the ability to keep itself alive[14].
Respiration
- Dyspnea is common as a person is dying. Being placed in semi-Fowler’s position can alleviate some pressure on their chest and make breathing easier. Additional oxygen can also be useful.
- The person may begin breathing with a wet sounding rattle called Cheyne-Stokes respiration; this occurs because mucus collects in the airway. A side-lying position, suctioning by the nurse, and mucus-reducing drugs can may be used to ease breathing.
- Air circulation is an important aspect of comfort. If a person is having trouble breathing, opening a window for fresh air or turning on a fan for increased circulation will help them breathe more easily.
Vision, hearing, speech
As a person approaches death, their vision, hearing, and speech systems will gradually fail.
- A person’s eyes stop working as they approach death. The person’s room at this moment should be well-lit but not bright; a dying person tends to turn towards sources of light.
- As a person progresses along their dying process, NAs must remember to verbalize their presence and their activities. Even if the person cannot respond, they are likely still hearing. Maintaining verbal communication with the person as they die is an important aspect of person-centered care, and may bring them comfort knowing that somebody is there with them.
- When speaking with the person, it is good to maintain a normal voice. NAs should not shout or whisper, but should instead engage with the person compassionately and under the assumption that the person can hear the NA and appreciates their presence and communication. NAs can use these moments to reassure the dying person and explain the care they are administering.
- A person will find it increasingly difficult to speak as they approach death. NAs should try not to put the person in a position of needing to provide long answers to questions, since this may be hard and exhausting if it is possible. NAs should do their best to anticipate the person’s needs; rather than asking “would you like your eyes cleaned,” NAs can notice when a resident’s eyes are gunky and can simply say “it looks like your eyes are uncomfortable, I am going to gently clean them for you with a warm cloth.” Similar approaches can be used for oral care, and for offering the person a bedpan.
It is necessary to maintain communication with the person, even if they are incapable of speaking or communicating. Since they can likely still hear, they may be calmed by knowing that care is being provided, or simply by the sound of another person’s voice. Something as simple as talking about one’s day or telling a story can help bring a dying person a moment of peace and distraction. What is one thing you could do or talk about to provide a dying person with a moment of comfort and connection? Write for 5 minutes, and share your response with a friend or classmate.
Nutrition and elimination
Nausea, vomiting, are common at the end of life. While nausea and vomiting can be mitigated using medications, loss of appetite is difficult to manage. NAs should never force somebody to eat or drink, as this will only make them more uncomfortable and emotionally distressed.
Some people may become too fatigued to eat and will require assistance, while others may simply refuse. Offering the person’s favorite foods in small, regular meals can stimulate appetite.
Urinary and fecal incontinence are common as a person is dying. So are constipation and urinary retention; NAs should report to the nurse if the person is showing symptoms for edema and constipation.
NAs will provide attentive catheter care according to the care plan.
The person may receive enemas to help ease their bowel movements.
The person and the family should have full control over how the person’s room is arranged. This helps the person and their family feel autonomous and in-control as they experience the end of life. Equipment that is unpleasant to look at such as suction machines, drainage containers, ventilators, and other devices should be removed or positioned out of sight of the resident. Personal items should be placed in view to help the person feel safe, peaceful, and at-home.
The family
A person’s family also goes through the stages of grief as their loved one is dying. This can be an extremely difficult time for family members and friends of the dying person.
NAs must provide close, attentive care to the person while also giving them and their family space to grieve and be together. NAs should be available, friendly, and courteous without imposing themselves on the family’s grieving process.
Some family members may want to participate in caring for the dying person. NAs should help family members care for the dying person, as long as it has been OK’d by the nurse.
Relationships with residents
NAs may develop close relationships with residents who are dying. Even if the NA feels especially close to the person, they should refrain from spending much time with the person while their family is present and instead focus on spending time with the person when they are not being visited by family and friends.
Be careful not to choose favorites among residents. Relationships are encouraged, because they genuinely improve a dying person’s quality of life. However, NAs should also remember that their care responsibilities extend to all patients they are assigned to, and that everybody deserves friendly companionship at the end of their life.
Legal and ethical concerns
There are certain legal and ethical issues at play when a person is dying or when they have already died[15].
Advanced directives
One important legal concept NAs must be familiar with is that of advanced directives. Advanced directives are instructions that the terminally ill person decides upon in advance should they die or become incapable of making or communicating their decisions (if they fall into a coma, for example).
Power of attorney, also called durable power of attorney or a health care proxy, is one form of advanced directive in which the dying person names another person as the arbiter of their medical care should they become incapable of making their own decisions. Power of attorney in this context only applies to what sort of care someone will or won’t receive; it does not entail anything about control over their finances or assets.
A living will is a document that details what sort of care the person does or does not want while they are still alive. A living will may instruct doctors not to use measures that prolong a person’s dying process, or to remove measures that prolong a dying process.
A Do Not Resuscitate (DNR) or “no code” order is put in place when the dying person decides that they do not want CPR performed on them when they go into cardiac arrest. When their heart stops beating, they want that to be their death; they do not want a healthcare team member to try to save them in that moment. Honoring DNR orders is an important part of respecting patient autonomy and empowering someone with agency over their own dying process.
The healthcare team needs to respect the wishes and autonomy of the dying person. It is critical that doctors and nurses take the time to fully explain the implications of advanced directives, and to follow up with the person to make sure they understand exactly what their choices are. Doctors and nurses are responsible for giving the person a realistic picture of what end-of-life treatment is and is not capable of doing.
Rights
 A person who is dying still has basic quality of life rights that must be upheld for all residents. People who are dying may find themselves dehumanized or objectified because of their proximity to death.
A person who is dying still has basic quality of life rights that must be upheld for all residents. People who are dying may find themselves dehumanized or objectified because of their proximity to death.
NAs must always respect the rights of people who are dying, and advocate on their behalf if they notice these rights being devalued or violated.
- The right to privacy before and after death. A person always has the right to ask someone to leave the room, including healthcare staff and visitors. A person also has a right to visit with others privately.
- A person should not be unnecessarily exposed to provide care, even after the person has died. Health team members must treat a person’s body with respect and dignity before and after the person has died.
- A person always has a right to freedom from abuse, mistreatment, and neglect. They also have a right to freedom from physical and chemical restraints, unless they become and active danger to themselves or others.
- Residents have a right to a safe and home-like setting. They should be encouraged to arrange the room in the way that makes them most comfortable, and to decorate the room with personal possessions that bring them comfort.
- The right to make choices extends to the right to refuse care; at a certain point, a person and their family may make the decision to refuse any further medical treatment. NAs and the rest of the healthcare team must respect this choice, even though it amounts to the person choosing to die.
Nearing death
The healthcare team, and the person themselves, may be able to tell when a person’s death is approaching. In the weeks leading to someone’s death, they may experience some or all of the following symptoms:
- Restlessness, agitation, and anxiety
- Depression
- Loss of appetite
- Nausea
- Dyspnea, shortness of breath, and pauses in breathing
- Drowsiness and persistent fatigue
- Confusion and disorientation
- Problems with elimination
- Swelling of the extremities and other areas
- Healing problems
- Changes in vital signs
- Diminished senses
The healthcare team may be able to tell when someone is about to die, or has just died. If NAs notice any of these signs they should alert the nurse immediately.
- Loss of movement, muscle tone, and sensation
- Abdominal swelling, vomiting, and involuntary emptying of the bowels and bladder
- The person’s measured body temperature rises, they feel cool to the touch with pallor, and have heavy perspiration
- The pulse becomes fast, weak, and irregular. Blood pressure will fall quickly.
- Slow or rapid respirations that give a “rattle” due to mucus in the airway
- A person’s pain decreases, and they may lose consciousness.
- When a person dies, they will have no pulse, no respirations, and no blood pressure. Their pupils will be dilated and fixed.
Postmortem
Postmortem care, or caring for the body of a person who has died, begins immediately after the doctor formally pronounces somebody as dead. A person’s family and friends may want to spend time with the body after their loved one has passed, either to process their own grief or two perform any religious or spiritual rites that they and the person deem necessary. NAs should be patient, kind, and present for family members grieving with a dead body.
Lecturio Nursing. (2022, October 19). How to Provide Postmortem Care After a Patient Death | Lecturio Nursing Clinical Skills [Video]. Youtube. https://www.youtube.com/watch?v=vtraSJQ6fsE
NAs provide postmortem care by turning off any machinery still hooked up to the person, and gently closing the eyes and mouth. Remember to provide for privacy, and to treat the body with gentleness and respect at all times.
NAs should position the body so it is properly aligned before rigor mortis sets in; rigor mortis is a stiffening of the body’s muscles that sets in 2 -4 hours after death. Once the body is properly positioned, NAs can gently sponge-bathe the body with the designated soap or cleansing agent. Drainage pads should be placed under the body’s head, buttocks, and anywhere else necessary to prevent leaking or mess.
The body should have a clean gown before being covered up to the neck with a sheet. Once the body is in good condition, visitors can enter and be with the body.
Once the visitors leave the body can be covered with a shroud, carefully transferred to a stretcher, and prepared for moving to a funeral home, morgue, or another location that prepares corpses for processing.
NAs should follow facility policy on cleaning the room and removing the person’s personal belongings after the body has been transferred.
Grieving
It is normal for staff members to grieve, especially if they were close with resident who passed. NAs should make sure to talk with friends and loved ones about their grief, and to do activities that allow them to emotionally and spiritually recharge.
If it seems like it would be helpful, NAs can share their grief with the person’s family, highlighting the positive experiences that the NA and the resident had together in the last stage of the resident’s life. The family may find comfort in knowing their loved one was cared for by somebody who saw their value and connected with them[16].
Key Takeaways
- Pain has a heavy impact on a person’s overall quality of life. Towards the end of life, pain presents an obstacle to a resident’s comfort, sleep, and wellbeing. Check in with residents about their pain levels, and communicate with the nurse about the frequency and quality of the residents’ pain. Provide a comforting presence and atmosphere whenever possible.
- Sleep is essential for comfort at the end of life. Make sure that residents have good opportunities for rest by providing a comfortable atmosphere, helping them with sleep conducive activities and nutrition, and scheduling care tasks around a resident’s uninterrupted sleep.
- End-of-life care is an important part of helping somebody die comfortably and with dignity. End-of-life care always involves a holistic approach, and tends to a person’s physical need for comfort, as well as their psychological, social, and spiritual needs as they approach death.
- The stages of grief are denial, anger, bargaining, depression, and acceptance. A person may not go through all of these stages in the grieving process, and will probably not go through them in a linear order. Understanding each stage of grief can help the care team work with a terminally ill person and their family to provide dignity and autonomy throughout their dying process.
Comprehension Questions
1) When is a person comfortable? Select the best answer.
a. When they are having their psychosocial needs fulfilled.
b. When they are resting well, and free from pain.
c. When they are free from pain and emotional distress, and the temperature is between 71- and 81-degrees Fahrenheit
d. When they are free from pain and emotional distress, have the full scope of their needs met, and have agency over their sensory environment
2) If a resident tells you that they are in pain, how should you respond?
a. Immediately tell the nurse that the resident needs pain medication
b. Ask questions about the pain to learn more about what might be causing it and how it can be treated; report the pain and what you learn about it to the nurse
c. Ask follow-up questions to make sure that the person is really in pain
d. Record that the person is in pain and ask if they need anything else
3) What are some details NAs should include in their observations about a person’s pain? Select all that apply.
a. Non-verbal behaviors like crying, gasping, or tightening facial muscles
b. What you think should be done about the pain
c. The location, duration, and intensity of the pain
d. Whether you think the pain is as bad as claimed
e. Any positions or activities that might have caused or worsened the pain
4) Beginning with hygiene care, what are some things NAs can do to help residents wind down in the evening and have a comfortable and restful sleep? Try to write about a paragraph with 5 – 6 details of the care provided.
5) Respond to the following sentences with T (true) or F (false).
____ Doctors can exactly predict when a person will die once they are diagnosed with a terminal illness.
____ A person’s attitude towards death will be influenced by their cultural, religious, and personal background. Nobody relates to death in exactly the same way.
____ People tend to have a more comfortable and dignified dying process when somebody else makes their practical decisions for them. This is to give them privacy and the space to introspect about their death.
____ Palliative care and hospice care are the same thing.
____ The number of people who use hospice services is increasing.
6) Please list the five stages of grief, and write a short description of each.
7) You are providing care for a dying resident named Ms. Haley. Even though she had been told she had weeks to live, Ms. Haley had been in good spirits until this morning. After breakfast, she yelled at you and blamed you for her illness. Rather than react, you try to comfort her, because you know that Ms. Haley is undergoing the grief process. Which stage of grief is Ms. Haley displaying?
a. Denial
b. Bargaining
c. Anger
d. Depression
8) As a person dies, their sensory systems will diminish and fail. Please describe two ways that NAs should communicate with a resident at this stage of their dying process.
9) Respond to the following sentences with T (true) or F (false).
____ A “DNR” order means that a dying patient does not want a defibrillator used; staff should use CPR instead.
____ Residents, or their power of attorney on their behalf, have the right to refuse care.
____ Residents who are dying are often the most shielded from abuse and negligence because they often have visitors.
____ As a person is about to die, their measurable body temperature falls and they become warm to the touch.
____ A person has a right to dignity and respect even after death. This matters for how their body is treated and handled.
10) What are some things NAs should do when providing postmortem care? Select all that apply.
a. Position the body in alignment and place any incontinence pads under the buttocks and had before bathing the body.
b. Allow the body to remain in the clothes the person was wearing when they died.
c. Immediately tell the nurse so any religious rites can be performed.
d. Have the family come in right away so they know what has happened.
11) Consider your own relationship to death and grief. How has your life experience shaped your relationship to death? How do you hope you will be able to relate to your own death when it eventually arrives? What is your experience or understanding of grief? What do you think it means to grief healthily, either for your own death or that of a loved one?
12) You have been able to form a friendship with a dying resident named Mr. Emma. Recently, Mr. Emma has started saying “I’m so scared of dying” every afternoon. What stage(s) of grief do you think Mr. Emma is experiencing? How could you converse with Mr. Emma in a way that provides comfort and allows him the space to work through some of his feelings? What questions might you use to start this conversation?
- National Institute on Aging. (2021, May 14). Palliative Care. National Institute on Aging; National Institutes on Health. https://www.nia.nih.gov/health/what-are-palliative-care-and-hospice-care ↵
- Nursing Assistant, Chapter 6 by Chippewa Valley Technical College is licensed under a Creative Commons Attribution 4.0 International License. ↵
- For information on the use of nonverbal pain scales, check out this video: https://www.youtube.com/watch?v=4uNnLd_oWf8. While the video focuses on juvenile patients, it is a useful introduction to utilizing non-verbal pain scales for people across the lifespan. ↵
- Centers for Disease Control. Tips for Better Sleep (2022). https://www.cdc.gov/sleep/about_sleep/sleep_hygiene.html#:~:text=Go%20to%20bed%20at%20the,smart%20phones%2C%20from%20the%20bedroom ↵
- Centers for Disease Control. Key Sleep Disorders (2022). https://www.cdc.gov/sleep/about_sleep/key_disorders.html ↵
- Sorrentino, S. A., & Remmert, L. N. (2019). Mosby's essentials for nursing assistants (6th ed.), Chapter 37. Elsevier. ↵
- Check out this resource for more information on different cultural and religious attitudes toward death: https://courses.lumenlearning.com/suny-nursing-care-at-the-end-of-life/chapter/diversity-in-dying-death-across-cultures/ ↵
- Heering, Helle, and Stephanie Gunder. “Spiritual Needs of Hospitalized Patients.” CINAHL Nursing Guide, edited by Diane Pravikoff, Dec. 2018. EBSCOhost, search.ebscohost.com/login.aspx?direct=true&db=rzh&AN=T700608. ↵
- QuickStats: Percentage of Deaths, by Place of Death — National Vital Statistics System, United States, 2000–2018. MMWR Morb Mortal Wkly Rep 2020;69:611. DOI: http://dx.doi.org/10.15585/mmwr.mm6919a4external icon. ↵
- Schub, Tanja, and Penny March. “End-of-Life Care and Decision Making.” CINAHL Nursing Guide, edited by Diane Pravikoff, Aug. 2017. EBSCOhost, search.ebscohost.com/login.aspx?direct=true&db=rzh&AN=T700310 ↵
- Dugan, D. (2020). Nursing assisting: A foundation in caregiving (5th ed.), Chapter 27. Hartman. ↵
- Kübler-Ross, E. (1969). On death and dying. New York, The Macmillan Company. ↵
- Family Comfort Hospice and Palliative Care. (2019, May 27). The Vital Role of the CNA in Hospice and Palliative Care. https://familycomforthospice.org/the-vital-role-of-the-cna-in-hospice-and-palliative-care/#:~:text=The%20Certified%20Nursing%20Assistant%20(CNA,palliative%20care%20team%2C%20is%20crucial. ↵
- Dugan, D. (2020). Nursing assisting: A foundation in caregiving (5th ed.), Chapter 27. Hartman. ↵
- Sorrentino, S. A., & Remmert, L. N. (2019). Mosby's essentials for nursing assistants (6th ed.), Chapter 37. Elsevier. ↵
- Check out this video for more information on caring for dying people and their families: https://www.youtube.com/watch?v=qaGVst-r50U ↵
Care given to make someone as comfortable as possible as they live with an incurable illness
A form of palliative care that is ordered at the final stages of a person's life
An approach to caregiving that conceptualizes it as caring for the whole person, in a way that prioritizes the person's agency and autonomy
Condition where a person cannot fall asleep or stay asleep
A disease or injury that will be the cause of someone's death
Directions given by a person that should be followed in a hypothetical future circumstance in which they cannot make decisions or communicate decisions about the care they want to or don't want to receive.
A power granted by a patient to another whom they trust to make decisions about their care and to advocate for them. Power of attorney does not automatically give someone power over another's finances or other matters.
An advanced directive that outlines the kind of care someone does or does not want, particularly when it comes to care that prolongs an inevitable death.
An advanced directive in which a person clarifies that once they go into cardiac arrest, they do not want CPR used to revive or save them.
Care provided to someone's body after they have died
A process 2 - 4 hours after death where a body becomes rigid and its muscles stiff
