12 Module 12 – Rehabilitative and Restorative Care
Rehabilitative & Restorative Care
Learning Objectives
- Demonstrate understanding of rehabilitative and restorative care
- Contrast reality orientation and validation therapy
- Demonstrate understanding of disease processes commonly requiring rehabilitation
- Apply effective communication techniques during the rehabilitative and restorative care process
The Focus of Rehabilitative & Restorative Care
Rehabilitative and restorative care aims to bring a person back to their normal level of functioning, or as close as possible to it, following an injury , illness, or medical intervention[1]. All of the Big Three should be considered in everything NAs do; when doing rehabilitative and restorative care, the emphasis will be on Resident Rights. We all have the right to regain and maintain our highest level of functioning. Care should always be given with this Right in mind.
Some helpful vocabulary:
- ROM: Range of motion (ROM) refers to how extensively a person can comfortably move different parts of their body
- ADLs: Activities of daily living (ADLs) are those daily tasks required for basic personal upkeep, such as bathing, dressing, and performing oral hygiene.
- OBRA: The Omnibus Budget Reconciliation Act of 1987 (OBRA) is a landmark piece of federal legislation that sets quality of care standards in healthcare facilities.
- Prosthesis: Prostheses are artificial replacements for a body part. Prostheses may be removable, such as a prosthetic arm, or irremovable, such as an artificial knee.
- Acute: Abrupt onset with a short course, such as an aggressive cold that has run its course in two weeks.
- Chronic: A disease or medical problem with a long course. When a chronic illness is under control it is in remission, while it is not under control then it is exacerbated. Chronic illnesses are usually not cured.
- Disability: Permanent or temporary loss of physical or mental ability and function.
- Atrophy: Loss of muscle tissue resulting from underuse.
The purpose
Rehabilitation and restorative care are necessarily holistic processes. This means that a person receiving care is understood as a whole person, whose care is not reducible to an isolated medical problem. Holistic care means that a person’s psycho-social, emotional, and spiritual needs are attended to, in addition to their basic physical needs.
Rehabilitation
Rehabilitation refers to the process of restoring a person to their highest level of physical, psychological, emotional, and economic function.
Part of holistic care is recognizing that all of these things go together; for example, if a person’s physical healing experience leaves them depressed and anxious, then the rest of their care will not go as smoothly and they may be less likely to report problems or seek medical care in the future. If the person is financially anxious and doesn’t have the tools to do effective financial planning, they may skip out on necessary care. 
NAs play an important role in knowing the people they care for, so they are able to report changes in their holistic wellbeing and get them connected with the team member best equipped to meet their needs.
Restoration
Restorative nursing care is the process that helps a person regain their holistic health, strength, and independence.
Image by Stannah International, CC BY 2.0.
Restorative nursing care involves caring for somebody on many different levels; for example, if a person leaves a facility technically healed, but with no confidence in their own ability to do something, then perhaps they had a need that was not effectively cared for.
Restorative nursing care aims to return a person to their regular level of functioning. Restorative care works to foster a person’s independence in all areas of life, including meeting one’s physical and psychosocial needs.
The team
It takes all of the many different roles on the rehabilitation team to care for someone holistically during the restorative nursing process[2].
- Physical therapists (LPT) work with the person to cultivate healthy, strong, stable, and pain-free mobility.
- Occupational therapists (OT) work with the person to promote independence and ability with the person’s ADLs, such as brushing their teeth, changing clothes, preparing meals, and socializing with others.
- Language and speech pathologists (LSP) work with the person on any issues that have with their mouth apparatus. Such issues may include difficulty with the mechanics of speaking, psychological and cognitive difficulties with language processing, and swallowing.
- Occupation therapy assistants (OTA) assist the OT, and physical therapy assistants (PTA) assist the PT.
- Registered nurses (RN) and licensed practical nurses (LPN) guide the nursing process by assessing the person’s ongoing needs, and providing and delegating holistic care.
- Rehabilitative and restorative aides (RA) are NAs who have received specialized training in restorative care.
- Medical social workers (MSW) perform a variety of roles such as advocating for the person in medical contexts, assisting them with discharge, and helping them achieve financial wellbeing and independence.
- Clergy and other religious figures can tend to the spiritual needs of a person. Residents have a right to spiritual care that accords with their religious and cultural background.
- The patient’s family and friends are a support system, a source of encouragement, and an important source of psycho-social fulfilment for the person. After the person is discharged, their family and friends will play an important part in the continuation of their restorative care at home.
Goals
The goals of rehabilitative and restorative care include fostering independence, promoting personal choice, providing opportunity for activity and exercise, and providing a safe environment.
Independence
Independence may look differently for everyone, though at a basic level it means being able to reliably meet one’s basic needs and safely perform ADLs. NAs can foster independence in ADLs by prompting the person to do as much of their ADLs unassisted, or with minimal assistance, as they can[3].
NAs can use verbal prompts and create a kind and supportive environment to help a person exercise their independence; for example, by suggesting that a resident change their clothing and brush their teeth, and then spend some time conversing with them while the resident performs these ADLs themself if they are able.
Promoting a person’s independence is important because it helps prepare someone for discharge and holistically fosters self-esteem.
Personal choice
A resident’s personal choices should be honored and encouraged at all times, as long as they are within the scope of the care plan. Residents have a right to make personal choices about what they eat, how they spend their time, who they spend time with, which doctors they see, etc.
These rights are legally protected and are part of a good care practice. Promoting residents’ personal choices is key to providing holistic, person-centered care.
Activity and exercise
Someone receiving restorative care will need to continue with as much exercise and activity as they can, as determined by discussions with the care team and the person’s care goals. Activity and exercise are important physically because they help prevent muscle atrophy; if a person remains immobile then they may experience complications across their bodily systems.
 Activity and exercise are important for promoting independence. Regular movement can make a person feel physically better and allow them to feel more capable. It can benefit their self-esteem, especially if improvements are made.
Activity and exercise are important for promoting independence. Regular movement can make a person feel physically better and allow them to feel more capable. It can benefit their self-esteem, especially if improvements are made.
Activity also promotes independence because a certain degree of mobility is necessary for independent living, and regular activity and exercise helps maintain mobility.
Image by eve.summermail is licensed under CC BY-NC 2.0.
Safety
The restorative nursing team must create a safe environment for a person to heal. A safe environment is one with minimal accident risks, and with an attentive care team to anticipate risk factors before they arise. A safe environment is also one where a person feels safe, and where their full spectrum of needs are met.

A safe environment…
- is one where the residents are physically secure from danger and risk of harm.
- is comfortable in terms of the sensory environment.
- requires that residents’ basic needs around nourishment, elimination, hygiene, and other ADLs are met kindly and promptly.
- includes privacy.
A safe environment is one where a person’s psycho-social and self-actualization needs are met. It will include ample time for socializing with the resident community, as well as encouragement for inviting visitors, family, and friends to come spend time with them. NAs can also help a resident fulfill their social and psychological needs by being an attentive listener, an enthusiastic conversation partner, and an enjoyable person to spend time around.
Restorative interventions
Independence, choice, activity, and safety will not be immediately attainable; they are goals that will need to be worked towards. Helping someone work towards independence in their ADLs demands strategic restorative interventions over time.
Examples of interventions include bowel and bladder training and incontinence measures, regular repositioning to prevent pressure ulcers, assisted ambulation to prevent atrophy and contractures, and assistance with nourishment.
NAs will need to closely observe people for signs of depression during the restorative care process. Rehabilitation can be difficult, painful, and socially isolating[4]. Depression is a common result. Signs of depression to watch out for include:
- social withdrawal
- appearing inattentive or vacant
- regular or excessive crying
- irritability and quickness to anger
- negative self-talk
- expressions of hopelessness
NAs should always provide a kind and encouraging presence to residents with depressive symptoms. If a resident is exhibiting signs of depression, NAs should document it and report it to the nurse so the care team can pay closer attention to the person’s mental healthcare and wellbeing.
Who needs rehabilitative and restorative care?
People across the lifespan require rehabilitative and restorative care for illness and injury. Some people need rehabilitative care in some form for their whole life, while for others it will be a temporary process. It is always emotionally taxing, and can even affect a person’s entire family.
The healthcare team is a provider of emotional and spiritual support, in additional to the physical and medical dimension of care.
An elderly person who has an accident, a bout of acute illness, or an exacerbation of a chronic illness may experience rehabilitative care differently than someone at other points of the lifespan. Older persons are more likely to have pre-existing co-morbidities and other conditions that may complicate or be complicated by their rehabilitative care.
Elderly people are at higher risk for injury both before and during the rehabilitative process; this means that they are more likely to need rehabilitative care in the first place, and more likely to experience a setback once they are there. Older adults heal more slowly than young people, so they will likely spend more time in rehabilitation than someone whose body heals quickly.
What does it mean to be independent?
Nobody is truly independent in the sense that we don’t need anybody else. We all rely on each other, and each of us has a need for care that make us inter-dependent with one another.
Restorative care aims to promote the best quality of life a person can have. A person’s independence should be encouraged up to the point where they reach their care goal, or where increasing their independence would not lead to their highest quality of life. A person has a right to their highest possible quality of life; they also have a right to the thoughtful and attentive care necessary to help them reach it.
The person and the healthcare team should remember that everybody has limitations, that personal and physical limitations are normal, and that there are ways to get human support and assistive devices to foster quality of life in ways other than promoting individual independence.
It can be helpful to think of “independence” and “dependence” as two poles of a very wide spectrum. Nobody is totally “independent” because we all need other people in order to have a high quality of life. Our place on the dependence – independence spectrum is not fixed; everyone will be more or less dependent on others at various points throughout our lives.
 It is important to remember that independence is a healthcare goal because it promotes a higher quality of life, self-esteem, and self-actualization, and not because individual independence is inherently a better way to live. Steps should be taken to promote a person’s independence by scheduling proper care and assistance, supplying appropriate assistive devices, and encouraging people to keep an active support system in place outside the facility.
It is important to remember that independence is a healthcare goal because it promotes a higher quality of life, self-esteem, and self-actualization, and not because individual independence is inherently a better way to live. Steps should be taken to promote a person’s independence by scheduling proper care and assistance, supplying appropriate assistive devices, and encouraging people to keep an active support system in place outside the facility.
Promoting healthy independence
NAs should always focus on a person’s abilities and strengths, rather than on the person’s perceived deficits. If a person can drink water on their own, but has difficulty with food, then the NA should encourage the person to drink on their own, assist as needed, and emphasize their capabilities and improvements.
“Maintaining activity levels” by Oregon State University, CC BY-SA 2.0.
Never encourage somebody to perform a task unassisted if unsure that the person can do so safely. If the person wants to perform a task unassisted that they usually require assistance with, the NA should stay with the person to make sure that they are safe and don’t require help during the task.
There are many different kinds of adaptive equipment that somebody can use to foster their independence. Mobility aids like canes and walkers, or special ergonomic silverware are just a couple of examples. Residents with trouble communicating may find assistive technology and text-to-speech software useful.
When obstacles to independence arise that cannot be managed with assistive devices, support systems should be in place to ensure the highest possible quality of life for the person even if there are some tasks they cannot perform on their own.
When is rehabilitative and restorative care necessary?
Rehabilitative care is necessary for a wide variety of conditions. In some circumstances, rehabilitation may be required for the foreseeable future or even a lifelong care need[5].
- Myocardial infarction (heart attack) requires ongoing rehabilitation such as a special diet, exercise, medication, and lifestyle changes like quitting smoking and regulating stress.
- Brain injuries require rehabilitative care because they often result in neurological complications that can impact things like ease of movement, speaking and eating, memory and executive function, and other activities that involve the nervous system.
- Spinal cord injuries require rehabilitative care, especially when they need surgery. Persons recovering from spinal cord injuries will need assistive with ambulation and elimination, amongst other things.
- Stroke recovery requires rehabilitative care because of the way a stroke can impact a person’s communication, eating, and movement.
- Chronic respiratory conditions require rehabilitative care in the form of respiratory therapy, lifestyle changes like quitting smoking, and additional oxygen.
- Fractures, joint replacements, and other musculoskeletal events require rehabilitative care to regain movement and manage pain.
- Severe wounds and burns may require rehabilitative care to regain mobility, manage pain, and control infection. Complicated chronic illnesses, such as diabetes, may also require rehabilitative care at different points along the disease process.
- Neurodegenerative diseases, or diseases that eat away at the brain over time like dementia, may require special rehabilitative care for people are too confused or disoriented to be cared for by family members or through home healthcare. Many facilities have specific memory care units for residents with neurodegenerative conditions that severely impact memory, orientation, awareness, and cognitive functioning.
Rehabilitation centers or floors can be found in hospitals, nursing homes and assisted living facilities, as stand-alone facilities, specific schools, and in home healthcare. Rehabilitative care will usually continue at home past the point of discharge – often, rehabilitative care is taken on by the person and their family, and maybe a home health aide[6].
Reality Orientation and Validation Therapy
It is important for NAs to keep the social and emotional needs of rehabilitation patients in mind. Requiring rehabilitative care can be disoriented, distressing, frustrating, and physically painful. NAs should always listen in an attentive and engaged way, ask follow up questions, and remain calm and positive while helping residents work through their feelings about the care process.
NAs can work to meet a person’s social needs by encouraging visitors, and promoting social relations amongst co-residents in a rehabilitation center.
Make the person feel as comfortable, safe, secure, and loved as they can. Everybody is worthy of care, respect, and security, and of being treated as an individual. NAs should check in with residents regularly to see if there is anything they need, and to just spend some extra time with them by telling them a story, writing them a kind note, and doing things that show the person they are not a burden and that they possess human value even when they do not currently have independence in most areas of their life. Such gestures of kindness will go a long way with anybody, but will be especially meaningful when somebody experiences disorientation, confusion, and loss-of-self that can come with neurodegenerative conditions.
Some people who require rehabilitative may be disoriented, confused, or cognitively impaired in some way. These limitations must be taken into account in communications in order to most fully meet the person’s social and emotional needs. Two different approaches to communicating with disoriented or cognitively impaired residents are “reality orientation” therapy and “validation” therapy.
“Reality orientation therapy” is a way of communicating with residents who are confused or disoriented in a way that attempts to orient them to reality. It is contrasted with “validation therapy,” which aims to communicate with residents in a way that affirms the world as they experience it rather than trying to correctly orient them to the external world.
Reality orientation therapy
Reality orientation therapy includes making sure that residents know their correct date, time, location, how to do their basic activities, and their name. It is important that residents are able to orient themselves to external reality in this basic way because it is a necessary step towards cultivating independence.
For example, if a person is having a bout of confusion and doesn’t know their own name then the NA should correct the them about their name. Similarly, if a person is confused about the date, day of the week, or what time it is, the NA should gently correct the person’s confusion in a kind and empathetic way.
If a person can usually perform one of their ADLs unassisted but seems to be having a bout of confusion, NAs should check in with them to make sure that they know how to perform the care task independently. If the person can verbally describe how to perform the task but still seems confused or disoriented, the NA should stay with them and observe just to make sure that the task is done safely and correctly.
Reality orientation therapy is appropriate when a person has temporary bouts of confusion and disorientation, and when they are not in a distressed or agitated state. Reality orientation therapy is especially appropriate when a person’s confusion and disorientation is a symptom of a condition where improvement and cognitive recovery are anticipated, though it can also be used in the earlier stages of dementia.
Psychosocial needs
Reality orientation, when it is effective, can help a person meet their social and emotional needs. Remaining oriented to a shared external reality, even if the person sometimes needs a little extra help orienting themselves to that shared external reality, is an important step in being able to socialize with people. It is useful for sharing information about oneself, discussing current events, showing interest in others’ lives, and other aspects of cultivating ongoing relationships with people in one’s community.
Reality orientation helps a person meet their emotional needs because being disoriented can be distressing and frustrating. Reality orientation therapy helps a person situate themselves with regard to a clearer and a more concrete version of their external reality.
Being oriented to a shared external reality can help a person understand their circumstances and regulate their emotions in response to their concrete environment.
Watch this video for some instructions on making an “orientation board.” Orientation boards can be helpful for residents who want a visual reminder of some key facts they can use to orient themselves.
Validation therapy
Validation therapy is different from reality orientation therapy, and requires training to utilize effectively. NAs should seek training on providing validation therapy if their facility offers it. If a person needs validation therapy it will likely be noted in their care plan.
Validation therapy involves meeting a confused or disoriented resident where they are. In other words, it means communicating with a disoriented resident from within their world, rather than trying to make them adjust their internal reality to fit the shared external reality. Practitioners “validate” the person’s experience, even if it is an experience that does not accord with their situation in the external world.
Under no circumstances should a person who requires validation therapy be corrected. Instead, they should be responded to in ways that work within their disorientation. For example, if a resident is convinced that he is late for work and needs to leave immediately, a validation therapy approach would be to ask why he is anxious to be on time. The goal is to let residents work through their feelings without imposing “reality” onto the resident; residents experiencing a misalignment between internal and external reality are often trying to process underlying feelings and experiences from their life.
Another example may be if somebody is anxious and worried that somebody is trying to find them. A validation therapy approach would not try to convince them that nobody is after them; instead, the response may be something like “the security in our building is good, and we are here with you. How can we help you feel safe?” This response does not explicitly affirm the resident’s experience, but tries to help ease the motivating emotion. Once they know that they are safe and listened to, the resident will be able to work through the underlying feelings behind their experience.
A another example may be that a resident is convinced a NA is their son or daughter. Rather than convince them that the NA is not part of their family, a validation therapy response may be to ask the person more questions about their children; help the resident feel what they are feeling in a safe and nonjudgmental way, without forcing them to relate correctly to their concrete external circumstances.
The goal of validation therapy is to make the person as comfortable as they can be, and to help them process whatever emotions they are feeling at the time. Validation therapy aims to calm the resident, without trying to make them feel or experience in a particular way.
TEDx Talks. (2015, June 3). Validation, communication through empathy | Naomi Feil | TEDxAmsterdamWomen [Video]. Youtube. https://www.youtube.com/watch?v=ESqfW_kyZq8
Always treat people with kindness, dignity, respect, and humanity no matter how disoriented or confused they are. Disoriented and confused residents are especially vulnerable to abuse, mistreatment, and neglect. If NAs see anybody acting abusively or neglectfully towards disoriented residents, they should alert the nurse immediately.
Disease processes commonly requiring rehabilitative care
Stroke
A stroke, or a cerebrovascular accident (CVA), occurs when the brain’s blood supply is cut off in an area, which causes the death of brain cells, brain damage, and swelling. Strokes can also occur due to a leak or a break in a cerebral blood vessel. Strokes that occur due to blocks in the brain’s blood supply are called ischemic strokes, while strokes caused by bleeding in the brain are called hemorrhagic strokes[7]. 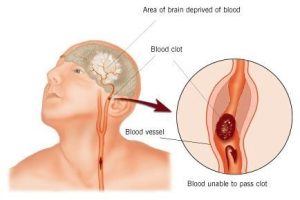
A person may be warned of an oncoming stroke when they experience a transient ischemic attack (TIA) brought on by lack of oxygen supplied to the brain. TIAs last anywhere from minutes to a full 24 hours.
Signs and symptoms of strokes and TIAs include:
- numbness
- paralysis and/or weakness on one side of the body
- confusion Image by ConstructionDealMkting, CC BY 2.0.
- issues with speaking and language comprehension (both spoken and written)
- vision loss
- severe headache
- problems with movement coordination, balance, and walking
If NAs notice a resident experiencing any of these symptoms, they should alert the nurse immediately.
Effects
The effects of a stroke can last a long time, sometimes for the rest of a person’s life. Rehabilitating and regaining functionality lost due to brain damage can be a difficult process and requires various therapies.
Effects of stroke include:
- loss of control in one’s facial muscles, extremities, and limbs
- hemiplegia
- a change in emotional makeup and personality
- aphasia
- changes in senses
- memory impairment
- bowel and urinary incontinence
- emotional impact such as depression as frustration with one’s circumstances
NAs will have to keep in mind that persons who have had a stroke will likely have a strong and weak side. Always take strong and weak sides into account when transferring somebody and helping them dress.
People who have had a stroke may have difficulty speaking and comprehending language. NAs should use their emotional intelligence to communicate with stroke victims. Patients with aphasia often have a difficult time accessing equitable care; they tend to have longer stays in hospitals, have less access to care, and promote frustration and dismissal from nursing staff due to their difficulties with communication[8].
Always practice patience with persons who have difficulties with communication, and follow the care plan put together in collaboration with the speech-language pathologist for communicating effectively with people who have had strokes, or suffer from aphasia for another reason.
Myocardial Infarction (heart attack)
Myocardial infarction is a dangerous medical event in which blood flow to the heart is suddenly blocked, causing a part of the heart muscle system to die.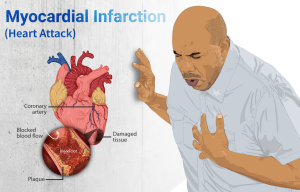 Heart attacks can occur for a variety of reasons, from vascular swelling, plaque build-up in the blood vessels, or because of embolisms or thrombosis[9].
Heart attacks can occur for a variety of reasons, from vascular swelling, plaque build-up in the blood vessels, or because of embolisms or thrombosis[9].
Symptoms of a heart attack include:
- chest pain and pain that radiates into the shoulders, neck, back and limbs
- heartburn
- dyspnea Image by Myupchar, CC BY-SA 4.0
- nausea
- dizziness
- sweating and clammy skin
- paleness
- sudden drop in blood pressure
- a weakened pulse
Symptoms may also be psychological, such as a deep existential fear and sense of doom, and an insistent denial of any heart problems.
In women symptoms can appear differently; women may have a myocardial infarction without experiencing chest pain, and instead will have pain across their body, nausea, dizziness and lightheadedness; symptoms of a heart attack in women can sometimes look like a sudden onset flu.
If NAs notice anybody experiencing these symptoms, they should make them rest comfortably and go get the nurse immediately.
Congestive Heart Failure (CHF)
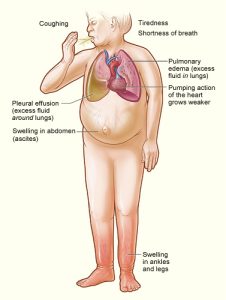
Congestive heart failure (CHF) occurs when one side of the heart loses its ability to effectively pump blood. CHF can occur as a result of heart damage from a previous adverse cardiac event, such as a heart attack, or may occur due to another cause like a degenerative disease. CHF occurs once the heart is too weak to adequately supply the body with oxygen and nutrients from the blood[10].
[11]Someone experiencing CHF will have fatigue, difficulty breathing, irregular pulse and heartbeat, edema, chest and abdominal pain, confusion, and difficulty exercising. NAs should report any changes in the condition of persons with CHF immediately, especially changes in their vital signs, urination, and fluid retention.
CHF usually impacts one side of the heart more severely than the other. The symptom profile of CHF changes depending which side of the heart is most severely impacted.
If the left side of the heart is failing, blood collects in the lungs because it cannot be transferred into the left side of the heart. This leads to orthopnea, weight gain, increased pulse, and coughing.
Right-side failure involves a collection of blood in the abdomen and lower extremities like legs and feet. This leads to edema in the feet and ankles, weakness, bulging veins (especially in the neck) and arrhythmia.
NAs should always follow the care plan exactly. Treatments for people with CHF usually include following a low-sodium diet to decrease water retention, providing additional oxygen, regular vitals, and daily weight observation. NAs should assist the person with activity and encourage them to rest, depending on what is stated in the care plan.
CHF patients will need meticulous intake and output recording, since they may also be on a fluid-restricted diet. NAs may want to keep the head of the bed raised at an angle to promote circulation. It is important to always follow the care plan, and to ask for clarification or assistance if unsure about anything.
Parkinson’s
Parkinson’s disease causes the progressive deterioration of brain tissue. The disease gets worse slowly over time, and there is no cure[12]. As brain tissue dies it can cause uncontrollable shaking and tremors, rigid and stiff muscles that impair mobility, slowed and uncoordinated movements, stooped posture, impaired balance, and mask-like facial expressions. Emotional and cognitive changes may also occur, such as mood swings, irritability, difficulty self-regulating emotions, memory loss, and disorientation.
NAs play important roles in caring for people with Parkinson’s. A person with Parkinson’s will have trouble controlling their elimination. NAs must practice attentive incontinence measures when caring for people with Parkinson’s by always answering their call lights promptly, practicing meticulous infection control and skin-care measures when episodes of incontinence occur, providing careful perineal care, and remaining positive and kind when assisting somebody with elimination.
Persons with Parkinson’s may need help with ADLs such as eating, bathing, and other self-care tasks. Lack of coordination and difficulties with movement can make ADLs difficult to perform unassisted. NAs should offer patient assistance, while allowing the person to perform the tasks they are able to do independently. Even if a person takes much longer to do a task unassisted, NAs should encourage them to do the task independently if they can and want to. Always maintain a person’s dignity and autonomy no matter how much help they need, or how long they take to perform their own care tasks.
NAs will need to assist people with Parkinson’s with ambulation and other tasks that require being upright. Safety measures must be taken to keep the person safe from falls and accidents. Always consult the care plan or the nurse with any questions about mitigating risk factors.
Dementia
Dementia is not a specific disease, but rather an umbrella term for groupings of symptoms such as amnesia, problems with communication and task completion, diminished coordination, impaired vision, and uncharacteristic behaviors. These symptoms result from brain damage caused by the buildup of protein cells, lack of blood supply, and nerve cell loss; the type of dementia that one has depends on what type of brain damage is occurring. Symptoms vary depending on what the damaged part of the brain controls.
The three most common types of dementia are Alzheimer’s disease, vascular dementia, and mixed dementia[13]. While a person can receive a general diagnosis of dementia, the more specific variant can only be determined by performing an autopsy. People with dementia often have more than one kind of dementia at one time. It cannot be cured or treated with medication.
Symptoms of dementia impact a person’s memories, abilities, language abilities, and personality.
Types of dementia
Alzheimer’s
Alzheimer's disease is caused by neurodegeneration resulting from protein buildup. It is the most common form of dementia; roughly 60 – 80 percent of dementia patients have Alzheimer’s. It primarily impacts people over the age of 65.
Alzheimer’s usually lasts roughly 8 years after the onset of symptoms, though it can last longer depending on age and overall health. Symptoms include progressive memory loss, confusion and cognitive dysfunction, difficulty with language and communication, and changes in personality and behavior.
Stages
There are three classificatory stages of Alzheimer’s. During the “early” or “mild” stage, the person experiences short-term memory loss and trouble recalling specific facts, confusion, and difficulty recognizing people and things. With some accommodations and forethought, someone at this stage can still lead a rather independent lifestyle.
The “middle” or “moderate” phase is characterized by a loss of independence and the need for consistent care and attention to ensure safety and wellbeing. Usually care at this level is given by family, community support networks, and in-home health or adult day services. Admission to a long-term care facility may be considered depending on the person’s symptoms and family circumstances. Memory loss continues to worsen, and more fundamental personality changes occur, and the person may lose the ability to remember how to dress themselves and perform other ADLs. This is usually the longest of the three stages.
The “late” or “severe” stage the person will lose all physical independence and will need 24-hour support care. Struggles with communication worse as language capabilities decline. Nutrition becomes difficult as the person forgets how to swallow, placing them at risk for choking and aspiration. Physical and cognitive cognition gradually worsens until they die. Care goals at this stage of the disease are not aimed toward promoting independence and instead seek comfort and a peaceful dying process[14].
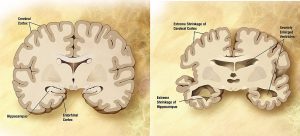
The brain
Alzheimer’s disease usually begins in the entorhinal cortex and the hippocampus, each of which play important roles in memory, task function, language processing, and sense of time. These parts of the brain are located in the temporal lobe, responsible for memory and general knowledge.
Roche. (2022, September). Science in Seconds | Chapter 2 | How does Alzheimer’s Disease change the brain? [Video]. Youtbe. https://www.youtube.com/watch?v=zB0dGQHTekg
Buildups of toxic protein molecules inhibit neurons from making connections. As the neurons die and more protein builds up, more and more areas of the brain experience damage. As different parts of the brain degenerate, existing symptoms worsen and new ones develop.
Eventually neurodegeneration impacts the cerebral cortex in other areas like the frontal lobe, parietal lobe, and occipital lobes. Damage to these lobes occurs in later stages of Alzheimer’s, although the progression of localized neurodegeneration depends on the type(s) of dementia present.
Frontal lobe damage results in impaired reasoning, issues with focus and task management, disinterest and lack of motivation, and problems navigating social situations. It also contains the motor cortex of the brain, which controls movement and tends to be damaged later during dementia progression.
The parietal lobes are located on either side of the brain, and control things like fine motor skills necessary for tasks such as putting on shoes or getting dressed. Parietal lobe damage is common in Alzheimer’s. Damage to the parietal lobes decreases a person’s fine motor skills, spatial awareness, and make coordinated tasks like writing difficult or impossible to accomplish.
The occipital lobe is located at the back of the brain, and usually degenerates later in the Alzheimer’s process. The occipital lobe acquires and processes visual information; deterioration of the occipital lobe can create difficulties with recognizing objects and understanding what they are for, navigating an environment, and with vision itself. Sometimes hallucinations occur[16].
Image by Cancer Research UK, CC BY-SA 4.0
Vascular dementia
Vascular dementia occurs when limited blood supply to the brain causes brain damage; it can occur gradually or after a sudden ischemic event. The specific sections of the brain that are impacted determine which symptoms present, and often result in difficulties with memory, language, walking, confusion, vision, and mental health[17].
The likelihood of vascular dementia increases with age as arteries are blocked by plaque or blood flow is reduced by vessels atrophying and becoming inelastic.
Mixed dementia
This form of dementia presents a wide mix of symptoms commonly associated with both Alzheimer’s and vascular dementia, and is caused by both protein deposits and poor circulation to the brain.
Communicating with and caring for persons with dementia
Persons with dementia experience problems with memory, confusion, and time orientation. These symptoms can lead to difficulties communicating with people and behaviors that caregivers may find challenging or disruptive.
Communicating with a person with amnesia and confusion can be challenging; caregivers should use specific strategies so as not to trigger feelings that are unpleasant or difficult to process. The most important thing is to always respond from a place of kindness and empathy; imagine what it would be like to not know where you are, or to believe you are somewhere that you are not. Always treat persons with dementia with respect, care, and dignity.
- When a resident repeats the same question over and over, respond with kindness and consider writing the information somewhere visible.
- If the resident searches for lost things, whether they ever had them or not, always show concern and help them search. It can be helpful to label the storage in a resident’s room so they know where to look for and put their objects, as well as labeling all personal objects.
- When a resident forgets the names of people or their relation, it can be helpful to slip it into conversation. Instead of saying “your visitor is here” you can say “your daughter Jackie is here,” or “Jason will be the person taking care of you today” even if Jason takes care of them every other day.
- If a resident tries to leave the facility to get home, distraction and diversion can be useful. Try to redirect the resident’s attention to an activity they enjoy in the facility, or come up with a reason why they must stay there, such as the weather or being on vacation.
- If a resident expresses a need to see a deceased loved one, invite them to talk about them as much as they want without confirming or denying that the loved one is alive. The more you know about a resident’s life, the more positive details you can draw their attention back to, such as their mother’s baking or their favorite activity to do with their spouse.
- Always speak in a calm and pleasant manner, and never allow annoyance or impatience to come through in your tone. Always speak in a way that conveys care.
Union Test Prep. (2018, May 14). CNA Skills: Caring For Dementia or Alzheimer’s Patients [Video]. Youtube. https://www.youtube.com/watch?v=QeaRogZQ-3Y
Challenging Behaviors
As the brain continues to degenerate, more challenging behaviors may appear. A challenging behavior refers to a behavior that poses a problem or an obstacle for a caregiver, such as an emotional outburst or resisting care.
Rather than engaging with these behaviors at face value, caregivers should always approach them from the perspective of their triggers and underlying causes.
- Emotional and behavioral outbursts are often caused by an underlying sense of frustration or fear.
- Aggressively resisting care can be caused by feelings of vulnerable insecurity or embarrassment, physical discomfort from the sensory environment, or something about the caregiver’s nonverbal communication or tone.
- Hoarding can be motivated by a fear of not having one’s needs met. Consider having the resident’s room cleaned at a time when they will be away, to clear away any stashed food. Make sure the person knows that they are being cared for, and that their needs won’t go unmet.
- Other behaviors such as pacing, wandering, or becoming especially confused in the late afternoons can be caused by lack of activity or stimulation, an unmet basic physical need of rest, nourishment, or elimination, or an unpleasant sensory environment.
Always take note of the conditions under which challenging behaviors arise. Reporting and recording as many facts about challenging behaviors as possible can help the care team notice patterns in the locations, times, and triggers of challenging behavior.
Always respond to challenging behaviors with calmness and compassion. Residents with dementia will pick up on and respond to tone and body language, so remaining calm is essential to the resident’s care and to your own ability to provide care. Do not react negatively to their behavior; instead, use redirection and distraction strategies[18].
Teepa Snow’s Positive Approach to Care. (2017, April 19). Challenging Behavior [Video]. Youtube. https://www.youtube.com/watch?v=ZpXeefZ2jAM
Resident Rights and Safety
Persons with dementia have a right to be treated with kindness, dignity, and empathy. If you notice any staff members interacting with residents with dementia in an unkind, uncaring, unprofessional, or abusive way, alert the nurse immediately. Always be conscientious and aware of your reactions and tone if you feel yourself becoming impatient with residents.
Persons with dementia often experience difficulty recognizing objects and navigating a spatial environment. An inability to recognize objects or sounds can also make a person feel unsafe – for instance, being startled and confused by a passing siren, or being unable to recognize chemicals or medication. Safety concerns should be anticipated in a person’s environment; hazardous chemicals, such as cleaning fluid and nail polish remover, medications, and any dangerous physical objects, such as a shaving razor, should be kept inaccessible to the person.
Fractures & Joint Replacement
Fractures and joint replacements are common in older populations due to frailer bone structures and diminished ease of movement. Older adults are more likely to fall or suffer another an accident that leads to a fracture. They may require joint replacement due to disease processes that impact joint health and functioning such as arthritis, or because of complications from injury[19].
Some older adults will require a total joint replacement, which is a surgical removal of the biological joint and replacing it with an artificial joint. The most common forms of total joint replacement are hip replacements and knee replacements.
- After a hip replacement surgery the doctor will decide how much weight the person will be allowed to bear on their new joint as they recover. NAs must carefully follow the care plan when it comes to activity levels, range of motion, and positioning following a hip replacement; abduction pillows may be used to keep the hips aligned in away that prevents the replaced joint from becoming dislocated.
- Knee replacement postoperative care requires the same level of attentiveness to the care plan as a hip replacement. Recovering from a knee replacement takes a long time, and is an extremely painful process. NAs should only perform range of motion and physical therapy exercises that are explicitly ordered; NAs should always follow the care plan exactly and ask questions if unsure.
- Persons recovering from joint replacement surgery should be encouraged to care for themselves, do things that make them feel good, and generally try to take their mind off the pain as much as possible. NAs can assist with this process by being positive and patient conversation partners, attending to the person’s needs promptly, and making sure they are eating and consuming enough fluids.
Excellent skin care and hygiene are essential when caring for somebody recovering from joint replacement surgery, since they will likely be totally or near-totally immobilized. Always follow the care plan with regard to positioning and activity.
If the NA observes signs of infection at the site of incision, changes in the person’s vitals, edema in the legs, skin discoloration, numbness, and or changes in the person’s vital signs, they should let the nurse know immediately.
Older adults are more prone to hip fractures; fractures are broken bones, and hip fractures are most often caused by a person falling and landing on their bottom or on their side. Hip fractures can sometimes heal on their own, or may require surgical interventions to heal properly.
Rehabilitation for a hip fracture can take up to 6 months, and comes with a variety of complications, many of them stemming from the immobility required for healing.
- Respiratory complications from immobility and reduced circulation
- People recovering from hip fractures are at risk of blood clots, especially in their legs. If the person reports pain in their calf or shortness of breath, the NA should report it to the nurse immediately.
- Persons recovering from hip fractures are at risk of developing immobility related complications such as UTIs, pressure ulcers, and constipation.
- Confusion, particularly in the geriatric population
People recovering from hip fractures will use a variety of assistive devices such as trochanter rolls and abduction wedges to position their body comfortably and safely. They will also likely use anti-embolism stockings to prevent blood clots in their legs, and raised toilet seats to help with elimination.
NAs should only use assistive devices as directed by the nurse; NAs play an important role in making sure that assistive devices are always clean and readily available, especially anti-embolism elastic stockings.
NAs should be extremely careful of the person’s body positioning and movements. Someone recovering from a hip fracture should not cross, bend, or flex their legs unassisted, and they should never be positioned as such. NAs must be vigilant and careful when repositioning and transferring residents, since twisting and pivoting motions can result in pain or other complications during the fracture healing process.
NAs should never perform range of motion exercises with somebody recovering from a hip fracture. They should make sure to always review the care plan, and to ask the nurse any questions regarding what should and should not be done with hip fracture patients.
Amputations
Amputations involve the full or partial removal of a body part, usually an extremity such as an arm or leg. Amputations are performed when a person needs a part of their body with cancerous tissue removed, or when tissue in a specific area dies. When localized tissue dies and begins to decay, it is called gangrene.
After amputation, the person may be fitted with a prosthesis. A prosthesis is an artificial body part of some kind. Dentures are a prosthesis.
Other forms of prosthesis include artificial eyes, arms, legs, hands, fingers, and more. Almost all prostheses are removable; NAs should pay careful attention when the nurse shows them how to properly attach and detach prostheses.
Sometimes a person with an amputation will experience phantom pain, or pain in an area of their body that is no longer there. Phantom pain can be caused by many different things, including damaged nerve endings and illness. Phantom pain is real pain; NAs should be sensitive to persons experiencing phantom pain, and alert the nurse when it occurs so they can explore options such as medication, physical therapy, and psychotherapy.
 Phantom pain is different from pain in the stump of the amputation; pain in the person’s healed stump may be caused by an ill-fitting prosthesis.
Phantom pain is different from pain in the stump of the amputation; pain in the person’s healed stump may be caused by an ill-fitting prosthesis.
NAs will need to provide emotional support to recent amputees. They should never indicate discomfort or disgust by the person’s stump, and should instead interact with it as they would with any other part of the person’s body. NAs should be positive and supportive as the person adjusts to their amputation or prosthesis. Receiving an amputation can induce anxiety, depression, frustration, and a sense of hopelessness. NAs should kindly and attentively listen to people, and remind them of their capabilities and human value.
“Kabul – prosthesis” by Barbara Millucci is licensed under CC BY 2.0.
Caring for recent amputees
The NA’s primary role in caring for a person who has received an amputation is to always follow the care plan when it comes to positioning, activity and range of motion exercises, and prosthesis care. Nurses will show the NA how to properly remove and attach the prosthetic; NAs should not handle prosthetics unless they have been trained to do so.
NAs must provide careful skin care for people with prostheses. When the prosthetic is removed at night, NAs should gently clean the stump area with a soap free of fragrance so the person’s skin does not become irritated. Perform other skin care around the prosthesis area as directed by the nurse.
If the NA notices any skin discoloration, redness or swelling, drainage or openings in the skin, or issues with the prosthesis they should alert the nurse promptly. They should also report and record any indications of stump pain or phantom pain from the person.
Hearing, Speech, and Vision Disorders
Hearing, speech, and vision problems may require rehabilitative care to heal the underlying cause, or to learn how to navigate the world with a different set of capabilities. Hearing, speech, and vision problems may be temporary due to illness, chronic disease, or physical accidents such as a brain injury. They may also be permanent and incurable, resulting from the aging process, injury, illness, or a congenital/birth defect.
Hearing, speech, and vision problems relate to all aspects of the Big Three, but they relate to Resident Rights most closely.  Residents have a right to know what is happening to and around them, and they have a right to be able to communicate effectively with the people who are providing their care. Facilities must have measures in place to accommodate the communication needs of residents with impaired hearing, speech, and eyesight. Residents also have a right to be able to communicate effectively with their family, friends, and other residents.
Residents have a right to know what is happening to and around them, and they have a right to be able to communicate effectively with the people who are providing their care. Facilities must have measures in place to accommodate the communication needs of residents with impaired hearing, speech, and eyesight. Residents also have a right to be able to communicate effectively with their family, friends, and other residents.
Hearing
The ear is made of the outer external ear which captures noise as vibrations, which are then carried and vibrate against the ear drum, which separates the outer ear from the middle ear. As the ear drum and three small bones in the ear vibrate in response to sound waves, it activates the cochlear nerve in the inner ear which translates those vibrations into the sounds that most humans consciously experience. In addition to hearing, the ear apparatus is responsible for helping humans maintain balance. Hearing loss is often accompanied by problems with balance and coordination.
Anatomy and physiology of the ear. (n.d.). Stanford Children’s Hospital. Retrieved May 31, 2023, from https://www.stanfordchildrens.org/en/topic/default?id=anatomy-and-physiology-of-the-ear-90-P02025
Hearing loss is a common problem across the human life span, though it is most common in older adults. Hearing loss is usually gradual, unless it results from an accident or an acute illness. Hearing loss may stem from an issue with the ear itself, or it can result from a problem with the brain or nervous system.
Hearing loss ranges from being very mild to total deafness. Someone experiences hearing loss whenever they are not able to hear a normal range of sounds. For example, not being able to hear high frequencies that most other humans can hear is an early indication of hearing loss.
Someone is considered “deaf” when it is impossible for them to understand speech just by listening to it. Deafness ranges from a person being able to hear some noises, to them hearing no sound at all.
Hearing loss can be caused by many different things. The most common causes of hearing loss are exposure to loud noises, and aging. Injuries to the ear or head that cause damage to any part of the ear or nervous system can also cause hearing loss. Tumors, hereditary characteristics, problems with circulation, chronic ear infections, and ear-wax build-up are other common causes of hearing loss.
Persons with hearing impairments have a wide variety of assistive devices they may have access to. The most common assisting device for those with hearing impairments is a hearing aid.  Hearing aids are small devices that are inserted into the person’s ear canal. Hearing aids are capable of amplifying sound, though they cannot genuinely improve a person’s hearing or language comprehension, nor can they make sounds clearer.
Hearing aids are small devices that are inserted into the person’s ear canal. Hearing aids are capable of amplifying sound, though they cannot genuinely improve a person’s hearing or language comprehension, nor can they make sounds clearer.
NAs should make sure that a person who needs a hearing aid is wearing it when they should be. NAs should always handle hearing aids carefully since they are fragile, expensive, and necessary for a person’s functioning and safety.
“Hearing aid” by Soitiki is licensed under CC BY-NC-ND 2.0.
Communication
Residents have a right to be able to communicate properly with healthcare staff, their friends, family, and visitors, and the other residents. When communicating with hearing impaired residents, NAs should keep a few basic strategies in mind.
- Eliminate background noises so the resident can focus on their interaction.
- NAs should always stand so the resident can see the NA’s face, watch their mouth, and read their body language to develop the clearest idea of what is being communicated.
- NAs should speak clearly, slowly, in a low pitch, and at a good volume without yelling. Using short and simple sentences, and somewhat exaggerated mouth movements, will help hearing impaired residents gather the meaning of the interaction. Sometimes cues will be appropriate, such as acting out taking a sip of water when asking the resident if they are thirsty and prompting them to drink fluids.
- NAs should keep a pen and a pad of paper available for communicating with hearing-impaired residents. This may be a person’s preferred way of communicating, or it may be their last resort. Either way, it is important to make as many resources available as possible to assist with communication.
Speech and language
Speech disorders impact communication and make speech and language difficult (without assistive devices) or impossible; some speech disorders only impact a person’s ability to form speech, while others impact a person’s ability to comprehend speech and/or language. Common causes of speech disorders include hearing loss, developmental disabilities and congenital conditions, and brain injuries and strokes.
Some different kinds of speech and language disorders include aphasia, apraxia, and dysarthria.
Aphasia refers to a total or partial loss of one’s ability to use and understand language. Aphasia is categorized as either expressive or receptive. Expressive aphasia relates to the way a person externalizes communication; a person with expressive aphasia will have difficulty expressing thoughts in language, whether verbal or written, though they may be able to comprehend language used by others.
Receptive aphasia relates to understanding language, or internalizing communication. A person with receptive aphasia will have difficulty comprehending language used by others, whether verbal or written. These two forms of aphasia are not mutually exclusive. When somebody experiences both forms of aphasia, it is called expressive-receptive aphasia.
Apraxia is a speech disorder relating to the muscles used for speech, rather than the comprehension of speech. A person with apraxia is unable to use their speech muscles to create understandable speech. This is due to damage in the area of the brain that controls motor speech. The person can understand speech, and knows what they would say if they could say it, but their brain cannot coordinate their speech muscles to make it happen. Apraxia deals with the capacity for speech itself, rather than the comprehension of language. A person experiencing apraxia can understand and create written language, whereas a person with total aphasia could not.
Dysarthria is difficult speech or speech that is hard to discern due to slurred words, speaking very slowly or softly, hoarseness, and drooling. Dysarthria occurs when a person’s mouth and facial muscles are affected by nervous system damage. A person with dysarthria will not have their language comprehension affected, but they will have a difficult time using their facial muscles to effectively perform verbal communication.
NAs must always be emotionally supportive, patient, and understanding when caring for people with speech disorders. NAs can be emotionally supportive even when a person is incapable of understanding language; communication occurs through body language, tone, eye contact, and various other ways of telling and showing a person that they are cared for and safe. When a person has a speech disorder that allows for some verbal communication, NAs must be patient and attentive and never become frustrated with the person, or frustrated with their own difficulty understanding the person.
SingHealth. (2022, January 17). Aphasia (Language / Speech Disorder) – CAREGIVER GUIDE [Video]. Youtube. https://www.youtube.com/watch?v=0gLbiHiGn80
NAs can communicate with people with speech disorders through consistent care and reliance on care routines and repetitive scheduling. They can also use a combination of emotional intelligence and consistency to devise ways of communicating; for example, when explaining a menu to somebody aphasia, NAs can use pictures rather than words to describe the dishes.
NAs should always treat adults with speech disorders as they would other adults. In other words, simply because somebody has difficulty making or processing language does not mean that they want to be infantilized or that they won’t recognize when somebody infantilizes them. NAs should remember that adults with speech disorders are humans with complex internal lives, and can be known and understood on a personal level even without conventional communication styles. .
NAs must always fully explain the care they are going to give before they give it. NAs must continue to communicate throughout the care process even when the person receiving care has inability or difficulty with comprehending speech. If the person is best communicated with in some other way, such as by writing or by gestures, then the NA should explain the care in the way that will be best understood by the person. This is absolutely essential in promoting Resident Rights and person-centered care.
The goal of speech rehabilitation is to improve the person’s ability to communicate. NAs should follow the care plan and therapies determined by the speech-language pathologist in collaboration with other members on the care team.
Speech rehabilitation works with the person to improve their affected language skills, use their remaining speech and language ability, and restore their language abilities to the highest possible extent. Other therapies involve muscle training to improve the person’s strength, coordination, and control of their speech muscles.
Speech-language pathologists will also work with the person to learn other methods of communicating. These other methods may involve strategies such as sign language, or include assistive devices such as text-to-speech and pictorial communication through a communication board. There is a wide variety of speech and language oriented assistive devices to make communication easier for those with speech impairments[20]; NAs should always closely follow the care plan, and familiarize themselves with any assistive technology used by those in their care.
Eye and vision
Eye disorders result in vision loss or impairment. Vision loss may be mild and partial, or it may be complete. Vision loss may be sudden or gradual, and occurring in just one or in both eyes. “Blindness” refers to the absence of sight, though somebody who is legally and functionally blind may still be able to make out vague shapes, colors, and light. Vision loss occurs due to a wide variety of causes, and can happen to anyone of any age, though it is most common in older adults.
Aging has notable effects on our vision and eye health.
UMass Memorial Healthcare. (2018, December 13). The effects of aging on our eyes [Video]. Youtube. https://youtu.be/MR9wZq4Hysg
Cataracts are a common vision problem that involve a clouding of the eye’s biological lens. Cataracts usually require surgical correction, in which the clouded lens is removed and replaced with an artificial lens.
Symptoms of cataracts include cloudy, blurry, or dimmed vision, faded colors, sensitivity to bright lights and presence of a glare, poor nighttime vision, the presence of halos around lights, and double vision in the impacted eye. Cataracts make it seem as if the person is looking through a waterfall, or always looking through a smudged pair of optical lenses.
Risk factors for cataracts are aging (the primary cause), a family history of cataracts (they are hereditary), diabetes, smoking tobacco, regular alcohol use, frequent exposure to direct sunlight, high blood pressure, and eye injuries and surgeries.
Glaucoma is a progressive disease where a person gradually loses their vision due to damage to their optic nerve. If left untreated, glaucoma will eventually result in blindness. Optical nerve damage is caused by pressure that builds up inside the eyes; onset of glaucoma can either be sudden, in which pressure causes substantial damage to the nerve quickly, or gradual, where damage occurs more slowly over time.
Glaucoma can occur in one or both eyes; if it occurs in both eyes, it may not affect each eye in the same way.
Glaucoma can be treated by surgery, medications, and anti-inflammation treatments. While glaucoma can be slowed and mitigated, there is not a known cure.
Ocular implants
Sometimes a person will need to have one of their eyeballs removed. If they decide they want one, they can be fitted with an ocular prosthesis, or an artificial eye. Some ocular prostheses are permanent implants, while others are removable. If the prosthesis is removable, the person will be taught how to remove, clean, and insert it on their own.
When caring for a person with an ocular implant, NAs must be extremely careful not to let the prosthesis become chipped, scratched, or damaged; always follow the care plan with regard to the storage and care of prostheses.
When communicating with people who have vision loss, NAs should always speak slowly, clearly, and directly face the person. NAs should knock before entering their room, as always, and carefully explain the care they are about to give before and during the care process.
Key Takeaways
- Rehabilitative and restorative care involves care that attempts to bring someone back to their highest available quality of life, independence, and capability. It involves care interventions that foster independence with one’s ADLs, implementing assistive technology, and putting a reliable support network in place.
- Reality orientation and validation therapy are two different approaches to communicating with residents who are confused or disoriented. Reality orientation therapy aims to help a confused resident orient themselves to the external world, particular their time, date, and location. Validation therapy involves providing a safe place for residents to work through their feelings without trying to correct them.
- Disease processes commonly requiring rehabilitation include cardiovascular diseases like heart attacks and CHF, musculoskeletal conditions or spinal and joint surgeries, and neurodegenerative diseases like Parkinson’s and dementia. Some diseases can be cured, while others are incurable and treatment only addresses symptoms. In either case, the goal of treatment is to return the resident to their highest available quality of life.
- Always be kind, patient, and attentive during the rehabilitative and restorative care process. Consider how a person’s limitations change the ways that they need to be communicated with. Good communication techniques are essential, and someone with dementia or impaired senses will need a considered and thoughtful approach to communication. Access to effective communication is a right.
Comprehension Questions
1) What is rehabilitative and restorative care?
a. A holistic, person-centered process of providing care interventions to promote a resident’s independence and return them to their highest quality of life.
b. A holistic, person-centered process in which NAs perform all of someone’s ADLs for them to allow them to rest.
c. A holistic, person-centered process to help someone get rid of addictive tendencies
d. A holistic, person-centered process to ease someone’s dying process
2) Residents receiving rehabilitative and restorative care may experience depression. Please list at least 3 and up to 6 symptoms of depression. What is one way that NAs can care for someone experiencing depression?
3) How can caregivers promote resident self-esteem and independence? Select any that apply.
a. When someone has difficulty or takes a long time with an ADL, caregivers should jump in and do it for them.
b. NAs can find assistive devices for things like combs and silverware to allow a person to groom or feed themselves for as long as possible.
c. Focus on what a person can do, rather than on what they cannot. For instance, if someone can wash their arms but not their feet, have them wash their arms and provide assistance with the feet.
d. Leave the room when a person is performing an ADL by themselves, so they know the staff is confident in them.
4) Respond to the following sentences with T (true) or F (false).
____ Reality orientation therapy aims to orient a resident to concrete features of their external reality such as the date, time, location, their name, and their ADLs.
____ Reality orientation therapy should be used for residents with late-stage dementia.
____ If someone responds to reality orientation therapy well, it can help them meet their psycho-social needs.
____ Validation therapy does not correct a confused resident, and instead aims to give them the space to process whatever feelings are motivating their particular confusion.
____ Validation therapy and reality orientation therapy techniques cannot be practiced together for the same resident.
5) Please list at least 6 and up to 12 symptoms of myocardial infarction. Indicate whether the symptom is experienced by only men or women, if relevant.
6) Which of the following diseases are neurodegenerative diseases?
e. Congestive heart failure
b. Dementia
c. Glaucoma
d. Parkinson’s
e. Arthritis
7) How should NAs provide care for someone with Parkinson’s disease?
a. Pay close attention for edema and swelling in the legs
b. Use distraction and redirection techniques in conversation
c. Attend to elimination needs immediately, and take extra measures to prevent falls and accidents
d. Take meticulous input and out recordings because of fluid restrictions
8) What is dementia?
a. Alzheimer’s disease
b. A mental illness
c. A group of symptoms caused by neurodegeneration
d. Caused by the buildup of proteins or vascular damage
9) Whenever you wrap your arms around a specific resident with dementia to secure a transfer belt, they seem surprised and try to hit you. This behavior happens with all their caregivers, which comes as a surprise because this resident is usually very nice and calm. You realize that being touched in this way is a(n) _____ of the challenging behavior.
a. Involuntary movement caused by brain damage
b. Trigger
c. Outburst
d. Result
10) Respond to the following sentences with T (true) or F (false).
____ Prostheses are artificial body parts, except for dentures and artificial eyes.
____ Phantom pain, as its name suggests, is not a real pain.
____ When communicating with a resident with impaired hearing it can be helpful to eliminate background noise and speak clearly face-to-face.
____ Verbal speech is the only form of effective communication.
____ A person with aphasia cannot understand communication in gestures and pictures.
11) The Big Three are important when caring for someone with dementia. Can you discuss how Resident Rights and Safety, in particular, are essential to keep in mind when caring for someone with dementia? Why might the rights of a resident with dementia be compromised by ineffective care? What would you do as a NA to keep someone with dementia safe and minimize the risk of accidents in their environment?
12) When a resident has dementia, it is important to interact with them from a place of kindness, compassion, and respect no matter how the resident is behaving. This is an obvious dimension of respecting Resident Rights. Why might paying attention to tone, body language, and strategic approaches to communication be important for your ability to provide any care in the first place? Consider the ways these things may impact somebody who is confused, afraid, and lacks impulse control.
- Nursing Assistant, Chapter 9 by Chippewa Valley Technical College is licensed under a Creative Commons Attribution 4.0 International License, except where otherwise noted. ↵
- Central Health. (n.d.). Restorative Care. Retrieved May 16, 2023, from https://www.centralhealth.nl.ca/restorative-care#:~:text=An%20interdisciplinary%20team%20consisting%20of,physical%2C%20social%2C%20spiritual%2C%20and ↵
- Nursing Assistant, Chapter 9 by Chippewa Valley Technical College is licensed under a Creative Commons Attribution 4.0 International License, except where otherwise noted. ↵
- Cairns, J. (2020, October 7). Percent of Residents Who Have Depressive Symptoms (Long Stay). Proactive Medical Review. https://proactiveltcexperts.com/percent-of-residents-who-have-depressive-symptoms-long-stay/ ↵
- Dugan, D. (2020). Nursing assisting: A foundation in caregiving (5th ed.), Chapter 25. Hartman. ↵
- Watch this video to hear the story of one person's long road to recovery after experiencing a traumatic brain injury (TBI): https://www.youtube.com/watch?v=FhegboT-FO8 ↵
- Center for Disease Control. (2023, May 4). About Stroke. CDC.gov. https://www.cdc.gov/stroke/about.htm#:~:text=A%20stroke%2C%20sometimes%20called%20a,term%20disability%2C%20or%20even%20death. ↵
- Hur, Y., & Kang, Y. (2022). Nurses' experiences of communicating with patients with aphasia. Nursing Open, 9(1), 714-720. https://doi.org/10.1002/nop2.1124 ↵
- Sorrentino, S. A., & Remmert, L. N. (2019). Mosby's essentials for nursing assistants (6th ed.), Chapter 33. Elsevier. ↵
- Malik A, Brito D, Vaqar S, et al. Congestive Heart Failure (Nursing) [Updated 2022 Nov 7]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK574497/. ↵
- National Heart, Lung, and Blood Institute, National Institutes of Health; Public domain
 ↵
↵ - National Institute on Agins. (n.d.). Parkinson's Disease: Causes, Symptoms, and Treatments. National Institute on Aging; National Institutes on Health. Retrieved May 26, 2023, from https://www.nia.nih.gov/health/parkinsons-disease#:~:text=Parkinson's%20disease%20is%20a%20brain,have%20difficulty%20walking%20and%20talking. ↵
- The American Red Cross. (2018). Excerpts. In Nursing Assistant Training (4th ed.) Chapter 20. https://www.redcross.org/content/dam/redcross/training-services/nat/Excerpts-from-textbook.pdf ↵
- The American Red Cross. (2018). Excerpts. In Nursing Assistant Training (4th ed.) Chapter 20. https://www.redcross.org/content/dam/redcross/training-services/nat/Excerpts-from-textbook.pdf ↵
- derivative work: Garrondo (talk)SEVERESLICE_HIGH.JPG: ADEAR: "Alzheimer's Disease Education and Referral Center, a service of the National Institute on Aging."PRECLINICALSLICE_HIGH.JPG: ADEAR: "Alzheimer's Disease Education and Referral Center, a service of the National Institute on Aging.", Public domain, via Wikimedia Commons ↵
- Alzheimer's Society. (2021, March). Understanding parts of the brain. alzheimer's.org.uk. https://www.alzheimers.org.uk/about-dementia/symptoms-and-diagnosis/how-dementia-progresses/parts-brain#:~:text=Damage%20to%20the%20parietal%20lobes,or%20writing%20much%20more%20difficult. ↵
- The American Red Cross. (2018). Excerpts. In Nursing Assistant Training (4th ed.) Chapter 20. https://www.redcross.org/content/dam/redcross/training-services/nat/Excerpts-from-textbook.pdf ↵
- The American Red Cross. (2018). Excerpts. In Nursing Assistant Training (4th ed.) Chapter 20. https://www.redcross.org/content/dam/redcross/training-services/nat/Excerpts-from-textbook.pdf ↵
- Nursing Assistant, Chapter 9, by Chippewa Valley Technical College is licensed under a Creative Commons Attribution 4.0 International License, ↵
- Check out this video for more information on augmentative and alternative communication (AAC) devices: https://www.youtube.com/watch?v=zmsdLzQW5G0 ↵
Caring for somebody healing from an injury or managing a disease in a way that helps them regain their highest possible quality of life
The full scope of a person's mobility. Range of motion exercises are ordered to regain or improve a patient's mobility and capacity for movement.
daily activities that a person needs to do to stay well, including daily hygiene, eating, dressing and undressing, and ambulating or other recreation
Also known as OBRA, this act set minimum quality of care standards in assisted living facilities
An artificial replacement for a body part lost to illness or injury
A disease that comes on quickly and lasts a relatively short duration
A disease that lasts a long time, and may be a lifelong condition
A condition in which a person cannot make full use of their body or environment in meeting the full scope of their needs
Weakening, shrinkage, and loss of ability
care that addresses the whole of a person, rather than just their illness
The methodical approach nurses use to determine the proper course of care and put it into practice
A heart attack. This occurs when the heart suddenly has severe issues with continuing to pump blood.
A stroke occurs when an area of the brain gets insufficient blood flow, interrupting its ability to function
Diseases like dementia and Parkinson's that corrode the brain's matter over time
Strategies for communicating with confused residents that attempt to correctly orient them to a shared external reality
A degenerative disease that damages the brain and affects memory, coherence, emotional regulation, motor skills and mobility.
Strategies for communicating with confused residents that help them process their feelings from within their own world, rather than imposing external reality on them.
Paralysis on one side of the body
Inability to form or comprehend language
difficulty breathing
A chronic condition in which one side of the heart loses its ability to pump blood effectively
Breathlessness while sitting, which is relieved when standing
The most common form of dementia
The part of the brain responsible for memory, task function, some language processing, and sense of time
Excessive collecting and guarding of objects and food
Stockings that apply even compression across the leg to promote healthy circulation
Dead tissue in a specific area
Difficulty coordinating speech muscles
Speech disorder in which a person's speech muscle control is impacted by damage to the nervous system
Clouding of the lenses in the eye
Progressive vision disorder in which vision is negatively impacted because of damage to the ocular nerve