9 Module 10 – Vital Signs
Vital Signs
Learning Objectives
- Understand the importance of vital signs
- Demonstrate proper technique in obtaining vital signs
- Demonstrate understanding of interpreting vital signs
- Develop understanding of cardiovascular and respiratory disease processes
- Demonstrate working knowledge of oxygen delivery
Vital Signs
Vital signs are measurements the healthcare team can take on a person that gives them key information on the functioning of a person’s key bodily processes like their blood and their breathing. The four basic vital signs are temperature, pulse, respiration, and blood pressure.
Vitals can help the team determine their illness, or the direction of their recovery. Vital signs can also be a general indication of health, or a sign that a patient is having a medical emergency.
Vitals measurements must be accurate, because they are important information for care planning, and give diagnosticians necessary information to make their diagnoses[1].
Temperature
The human body only functions properly within a specific temperature range. Temperature refers to the amount of heat in the body. While the body has its own means of regulating temperature, but sometimes the balance between heat produced and heat lost tips into an unhealthy range.
Standard average body temperature for a human is about 98.6 degrees Fahrenheit, though it fluctuates depending on how the measurement is taken. Normal temperature range is considered to be 97 – 99 degrees Fahrenheit.
Body temperature is affected by multiple factors such as age, exercise, stress, illness, and medications
- Age impacts body temperature due to associated loss of fatty tissues and diminished blood circulation.
- Exercise increases body temperature as muscles produce heat during activity.
- Stress can increase a person’s body temperature because of hormones like adrenaline, cortisol, and epinephrine. The human body’s temperature responds to its hormonal state.
- Illness can increase a person’s body temperature either due to a symptom of the illness or as a result o
f fever.
- Drugs such as Tylenol, aspirin, and ibuprofen are considered fever-reducing drugs because they lower body temperature. Somebody is only considered “fever-free” if their body temperature stays within a normal range without the use of fever-reducing medication.
Sebastian Porta, Cory Kontros, Andrew Starr-Bochicchio, CC BY-SA 3.0
Taking someone’s temperature
A normal human temperature range is 97 – 99 degrees Fahrenheit. Subnormal body temperature could be caused by exposure to cold, alcohol use, illness and infection, and other factors.
A person has hypothermia when their body temperature is too low to permit normal functioning. Symptoms of hypothermia include cyanotic skin (pale and blueish in color), numbness, shivering, impaired breathing, slowed movement, and confusion and disorientation. If any of the symptoms are observed, alert the nurse.
A person’s temperature can be taken in different ways, and each method will have slightly different normal ranges. Always practice Standard Precautions while taking someone’s temperature by wearing gloves and other PPE as required. The most common methods of taking someone’s temperature are the oral, rectal, tympanic, and axillary[2].
Oral temperature
Oral temperature is taken from the mouth, and is usually taken with a digital thermometer. A normal temperature range for most oral thermometers is 97.6 – 99.6 degrees Fahrenheit. Eating or drinking, smoking, or exercising within 30 minutes prior to taking oral temperature can produce an inaccurate reading.
After performing the opening procedure, the NA should remove the thermometer and put on the plastic sheath. Put it in the person’s mouth to one side after instructing the person to hold the thermometer in their closed mouth.
When the thermometer indicates that it has read the temperature the NA should commit the number to memory before taking the thermometer from the person, discarding the sheath, and cleaning the thermometer in accordance with facility protocol.
Wait with the person and not leave the room while an oral temperature reading is being taken. The process is finished after recording the temperature and performing the closing procedure.

Image marked with CC0 1.0.
Rectal temperature
Rectal temperature is taken by inserting a thermometer ½ to 1 inch into a person’s rectum; a normal temperature range for a rectal reading is 98.6 – 100.6 degrees Fahrenheit. A person may need their rectal temperature taken if they cannot use an oral thermometer.
A person may be uncomfortable having their temperature taken in this way, so NAs should be respectful and explain the process thoroughly. The person must hold still during the temperature reading, so their being calm and cooperative is essential for taking accurate vital measurements.
To take someone’s rectal temperature NAs should always begin with clear and calming instructions on how the person needs to cooperate by sitting still during the process in order to get an accurate reading. Provide privacy when someone is exposed by closing their door and privacy screen.
NAs should prep the thermometer by lubricating the tip or applying a cover for the probe. Rectal thermometers look similar to oral thermometers. Once the thermometer is prepped and the person is positioned in left-lying Sims’ with only their buttocks exposed, the thermometer tip can be inserted ½ to 1 inch in the person’s rectum.
Never force an object into someone’s rectum; if the thermometer encounters resistance, the NA should stop. The person’s buttocks should be covered again while the thermometer gets the reading; the NA must hold onto the thermometer at all times.
After recording the temperature, clean the thermometer according to facility policy.
Tympanic temperature
Tympanic temperature is a temperature reading taken from the person’s ear canal. A normal reading for tympanic temperature is between 96.6 and 99.7 degrees.

After preparing the thermometer, gently position the person’s head right in front of them and straighten the ear canal by tenderly gripping the outer edge of the ear at about 11 o’clock, and pulling it up and back. Tympanic thermometers should only be inserted about ¼ to ½ an inch into the ear canal.
Keep holding the ear and the thermometer until the thermometer is finished with the reading. The reading should be memorized immediately.
After committing the reading to memory, Image by wuestenigel, CC BY 2.0 the NA can clean the thermometer or discard the disposable sleeve, discard gloves and wash hands, and record the person’s temperature on their chart.
Temporal temperature
A temporal thermometer is a non-invasive thermometer that takes a person’s temperature by being swiped across their forehead. It is especially useful for children, and people who require a noninvasive approach. A normal reading for a temporal thermometer falls between 97.6 and 99.6 degrees Fahrenheit.
Axillary temperature
Axillary temperature is taken at the person’s armpit. While this method is less accurate than oral, rectal, and tympanic temperature, it is also safer and less invasive than methods that require inserting a thermometer into an orifice. A normal range for axillary temperature is between 96.6 and 98.6 degrees Fahrenheit.
When taking a person’s temperature always perform the opening procedure and allow for privacy. Once the thermometer has been prepared, help the person remove their arm from their sleeve and tuck the thermometer into the person’s armpit. The person should hold their arm close to their chest to keep the thermometer in place. The reading will take between 8 and 10 minutes.
Once the reading is complete the NA should commit the number to memory before discarding gloves and washing hands, and helping the person get re-situated in their clothing. The temperature reading should be recorded immediately along with the method used to take it.
Pulse
The heart
The three vital signs other than temperature (pulse, respiration, and blood pressure) all closely involve the circulatory system. In other words, a person’s vital signs closely relate to the workings of their heart. A person’s heart is located on the right side of their chest and is about the size of a fist. The heart is made of muscle tissue and, through its contractions, is responsible for the movement of blood throughout the body. The heart pumps about 7,000 liters of blood through the body every day.
FuseSchool – Global Education. (2017, April 6). Heartbeat and Pulse | Physiology | Biology | FuseSchool [Video]. Youtube. https://www.youtube.com/watch?v=DLmmN0jy-s0
The heart consists of four hollow chambers; there are two atria, which fill with blood before being pumped to other areas of the body, and two ventricles, which pump blood to the lungs, head, and all the way to the feet. When the heart beats it makes a lubb-dubb sound.
The “lubb” part of that sound is the systole, or the part of the heartbeat when the heart contract and makes the motion that pumps blood. The diastole is the “dubb,” or the part of the heartbeat when the heart relaxes, refills with blood, and prepares to make another contraction. During diastole, blood from the atria flow into the ventricles before being pumped to other parts of the body.
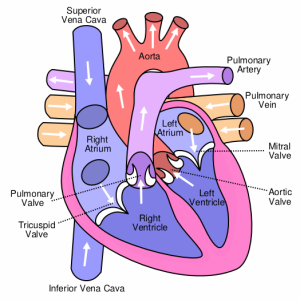
created by Wapcaplet, CC BY-SA 3.0
Measuring pulse
Pulse is an important vital sign that will need to be measured regularly. Pulse refers to the rhythm of blood moving against an arterial wall, and is measured as “beats per minute” (BPM). Pulse can be measured in many different areas on the body, technically anywhere an artery is close enough to the surface of the skin for a person to feel the rhythm of blood.
The normal range for pulse in adults is 60 – 100 BPM, with most adults averaging about 70 – 80 BPM. When counting a person’s pulse, in addition to counting BPM, NAs should pay close attention to the rhythm and force of the beats[3]. A pulse’s rhythm should be regular as in the time between beats is roughly equal; a pulse should feel strong but not thumping.
When taking a radial pulse, the NA should gently and firmly place two fingertips on the thumb side of the person’s inner wrist. The person may also appreciate some extra support to support their arm and hand. Count each pulse beat for exactly 30 seconds. However many beats the person’s pulse has in 30 seconds should be doubled to find the beats per minute. If the pulse is irregular then the NA should count the pulse for the full 60 seconds.
The apical pulse is taken for a full 60 seconds and is located on the left side of a person’s chest, just below their nipple. Apical pulse is used for persons with irregular heart rhythms, heart disease, and heart medications[4]. The apical pulse is taken using a stethoscope; NAs should make sure that the earpiece and diaphragm (flat piece placed in contact with the person whose pulse is being taken) of the stethoscope have been wiped off properly before use. The stethoscope should also be cleaned after use.
The apical-radial pulse is a way of measuring pulse that takes both the apical and radial pulse into account. Counting an apical-radial pulse will require two people, one to take the apical pulse and one to take the radial pulse. The apical pulse is usually either the same or higher than pulse taken at other areas of the body; if the apical pulse is lower than pulses elsewhere, it is an indication of very poor circulation. When the apical pulse is higher than the radial pulse the difference is called the pulse deficit.
https://www.youtube.com/watch?v=yhoi2nVE9o8
Skills Lab. (2017, August 20). B 804 Assessing apical-radial pulse [Video]. Youtube. https://www.youtube.com/watch?v=yhoi2nVE9o8
Blood pressure
While pulse is the rate at which blood is pumped through veins and arteries, blood pressure refers to the amount of force exerted upon the walls of an artery by the blood. A person’s blood pressure is determined the amount of force with which the heart contracts, the amount of blood pumped with each heartbeat, and how easily and smoothly the blood is able to flow through the blood vessels.
Blood pressure readings are recorded as the systolic blood pressure over the diastolic blood pressure; they look like a fraction, such as 110/70. The top number, systolic pressure, measures the force of blood as the heart contracts, while the lower diastolic number measure the force of blood as the heart is at rest in between lub-dubs. The normal range for systolic blood pressure is 90 – 119, while the normal range for diastolic blood pressure is 60 – 90.
Hypo- and hypertension
Hypotension is the word for low blood pressure. A person is considered hypotensive is their systolic blood pressure falls below 90 or their diastolic blood pressure falls below 60. Postural hypotension is a common form of hypotension where a person experiences a sudden drop in blood pressure when they stand or sit up quickly. A person with postural hypotension may become lightheaded, dizzy, or event faint if they stand or sit up quickly.
Hypertension is high blood pressure. Hypertension can be dangerous in its own right, and is a symptom of many different heart conditions and circulatory problems. There are a few different classifications of high blood pressure[5].
- Elevated: Systolic pressure 120 – 129 and diastolic less than 80
- Stage 1 of hypertension: Systolic 130 – 139, or diastolic 80 – 89 (only one needs to be present for classification)
- Stage 2 of hypertension: Systolic pressure 140 or higher, or diastolic 90 or higher
- Hypertensive crisis: Systolic pressure 180 or higher, and/or diastolic pressure 120 or higher. A person in hypertensive crisis will require immediate emergency medical services.
Hypertension is widely known as the “silent killer.” Hypertension can develop in people of any age, and is diagnosed when a person’s blood pressure is regularly above 130 (systolic) and/or above 80 (diastolic). Symptoms of hypertension include headaches, dizziness, and blurred vision.
Long-term hypertension usually occurs when a person’s blood vessels harden and narrow; it can also be caused by high levels of stress and pain, arterial plaque buildup, as a side effect of medications, and other factors.
Hypertension can lead to heart attacks, especially when it is related to a blockage of a blood vessel, also called an occlusion. Occlusions can cause ischemia, which is when an area does not get sufficient blood supply, which can also lead to a stroke.
NAs will need to take frequent blood pressure readings on people with hypertension to closely observe and record any abnormally high readings or sudden changes from the person’s usual readings.
TED Ed. (2015, July 3). How blood pressure works – Wilfred Manzano [Video]. Youtube.com. https://www.youtube.com/watch?v=Ab9OZsDECZw
Measuring blood pressure
Blood pressure is measured using a tool called a sphygmomanometer. Sphygmomanometers are either manual or digital. To take someone’s blood pressure, the NA will need the sphygmomanometer, a stethoscope (only if using a manual sphygmomanometer), a blood pressure cuff, and alcohol wipes.
Sphygmomanometers are made of an armband that tightens either through the manual use of an attached handheld squeeze-ball air pump or the arm band will tighten automatically, as well as an interface where the blood pressure is displayed, and tubing that connects the arm band with the display.

“sphygmomanometer” by kndynt2099 is licensed under CC BY-NC 2.0.
A person’s blood pressure should not be taken if they have recently engaged in activities that raise or lower their blood pressure. Examples include exercise within the last 30 minutes, and the presence of caffeine, tobacco, and other drugs.
Be careful of placement when taking blood pressure. The sphygmomanometer’s arm band should not be placed on an arm that has an IV line, a cast, burns or injuries, recent physical trauma, a mastectomy or another surgical incision on that side, or dialysis treatment. Arms that are paralyzed or have been amputated should not be used to measure blood pressure.
Taking a person’s blood pressure manually requires substantial concentration and focused listening. After performing the opening procedure and cleaning the equipment, discuss the procedure with the person and ask them to cooperate by remaining calm, quiet, and still.
After making sure the cuff is completely deflated, the NA should wrap the blood pressure cuff around the person’s bare arm positioned palm-up at about heart level, with the cuff’s center placed about 2 inches over the inside of the elbow.
Place the stethoscope over the artery on the inner elbow and tighten the valve on the arm cuff until it is closed but not too tight. Use the handpump to inflate the cuff to 170 – 200. The valve should slowly be opened until a pulse beat is heard; if a pulse is heard immediately at the original number, deflate and begin the process at a higher pressure.
Listen carefully while deflating the cuff. The number on the gauge when the first pulse becomes clearly audible is the systolic blood pressure and the first number in the reading. The gauge reading when the pulse beat sound changes or disappears is the diastolic blood pressure. Once the diastolic pressure is observed the NA can fully release the cuff valve before removing it. The systolic and diastolic numbers should be recorded immediately after handwashing. If the reading is abnormal or a significant change from other readings, inform the nurse.
Obtaining a blood pressure reading on someone is much simpler with an automatic sphygmomanometer than with the manual variety. After performing the opening procedure, the NA should make sure the cuff is totally deflated before positioning it so the center is right above the brachial artery. The cuff should be snug. Next, turn on the blood pressure machine and select the proper settings. After the machine performs the reading the NA should chart the blood pressure immediately and details like the arm used and the time the measurement was obtained.
RegisteredNurseRN. (2019, June 4). Blood Pressure Measurement: How to Check Blood Pressure Manually [Video]. Youtube. https://www.youtube.com/watch?v=UGOoeqSo_ws
Respiration
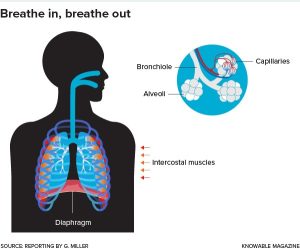
Respiration is the process of breathing, or moving air into and out of the lungs. Our lungs extract the oxygen from the air and use it to replenish the oxygen in our blood. Respiration occurs in two parts; we inhale during inspiration, and exhale during expiration; a full respiration is both an inspiration and expiration, or one breath in and one breath out. The normal rate of respiration for adults is between 12 and 20 breaths per minute[6].
Nobody breathes in exactly the same way, however in general a person’s breathing should be effortless and quiet. Occasional sighing is normal, though if sighing is consistent and regularly it could be a sign that they are breathing too shallowly.
When a person breathes it activates their diaphragm, a small and powerful muscle beneath the lungs, and the intercostal muscles, which are the three layers of muscle tissue between the lungs and the ribcage. As inspiration occurs the muscle system expand and makes space for the inflating lungs, and upon exhalation the muscles contract and help to squeeze the leftover carbon out of the molecules. The bronchiole carry air to the alveoli, which help oxygen enter the blood stream.
Measuring respiration
NAs can obtain a count on a person’s respirations during the same process as getting their radial pulse. After the first 30 seconds spent taking a person’s radial pulse, the NA should keep their fingers on the person’s radial pulse while switching to counting their breaths for the next 30 seconds.
A person’s respirations often change when they know that their breathing is being observed. Instead of explicitly telling them, transition right from taking a person’s radial pulse to counting their respirations by observing or feeling the rise and fall of their chest. Respirations can be counted for 30 seconds and then multiplied by two to obtain respirations per minute; if breathing is irregular, respirations should be counted for the full 30 seconds. Image by knowablemag is licensed under CC BY-NC-ND 2.0
Observing respiration
Closely observe a person’s breathing for signs of irregularity and difficulty. If a person experiences apnea, the temporary absence of breathing, or dyspnea, labored or difficult breathing, they should alert the nurse immediately.
Other symptoms of breathing problems include:
- irregular breathing or changes in breathing rhythm
- weak or shallow breathing
- breathing noises such as gurgling, wheezing, snoring sounds, grunting, etc
- use of shoulders and chest during respiration
- breathing abnormally fast or slow
- skin and lip discoloration
Problems with a person’s breath often result from or precede an adverse medical event, and must be reported immediately.
Vital sign review
RegisteredNurseRN. (2019, May 13). Vital Signs Nursing: Respiratory Rate, Pulse, Blood Pressure, Temperature, Pain, Oxygen [Video]. Youtube. https://www.youtube.com/watch?v=gUWJ-6nL5-8&t=23s
Oxygen Delivery
What is respiration?
Respiration is the process of gas exchange between a person and their environment; the human body takes in oxygen from the environment, removes the oxygen to fuel its blood and cells, and then expels carbon dioxide back into the environment. The average adult takes about 20 breaths per minute.
The lungs are where blood exchanges carbon dioxide waste from the body’s cells with fresh oxygen to re-supply the cells with energy. The blood then transports oxygen throughout the body, while removing carbon dioxide from our cells and taking it back to the lungs to be disposed of. The body naturally strived for balance in oxygen and carbon levels, and when the balance is tipped someone may start to breathe irregularly in response.
Medical Animation Videos. (2014, February 4). Gas exchange in lungs physiology
video animation – made easy [Video]. Youtube. https://www.youtube.com/
watch?v=AJpur6XUiq4
Factors impacting oxygen delivery
Different factors impact a person’s oxygen needs and ease of respiration. A person’s oxygen needs are impacted by their overall respiratory health; how wide and clear the airways are, levels of inflammation, and the health of the person’s lungs and air sacs all contribute to oxygen needs[7].
Circulatory health: The circulatory system delivers the oxygen to the rest of the body. Blood vessels must be open and flexible enough to deliver large amounts of blood to every area of the body. Capillaries are tiny blood vessels that widely distribute blood throughout the body including the areas that don’t have large blood vessels, such as our fingers, ears, and scalp. Capillaries are everywhere, are about the thickness of a small hair, and have extremely thin walls to promote the exchange of fluid, gas, and nutrients between blood vessels and other tissues.
As a person ages their blood has a lower red blood cell (hemoglobin) count. Red blood cells carry the oxygen to different parts of the body. The fewer red blood cells a person has, the less effective will their oxygen delivery system will be.
As a person ages their blood vessels become stiffer and inelastic, which also inhibits oxygen delivery.
Exercise: When a person exercises their body uses much more oxygen than when it is at rest. Exercise can have a positive impact on a person’s oxygen delivery system by expanding lung capacity and widening blood vessels, or a negative one by worsening symptoms of respiratory conditions such as asthma.
Nervous system is also involved in respiration; the nerves throughout our body send signals to our brain when our oxygen needs change and when something is wrong. Impairments to the nervous system can impact a person’s breathing. For example, if somebody is paralyzed from the neck down they may require an assistive device to continue delivering oxygen.
Aging: Lung and respiratory muscle strength diminish with age, and lung and airway tissue loses elasticity.
Environment: The particulate content and air quality of the air a person breathes can cause negative side effects. Persons who smoke cigarettes, especially if they’ve been smoking for a long time, will have harmed their respiratory system. Environmental pollutants can have a harmful impact on a person’s ability to breathe well. Seasonal or environmental allergies have a negative impact on a person’s respiratory system when the allergen is present, sometimes causing airways to swell and close, or causing breathing to be interrupted by severe congestion.
MotivationalDoc. (2015, December 6). Proper Breathing Exercise to Strengthen Lungs to Keep Healthy – Dr Mandell [Video]. Youtube. https://www.youtube.com/watch?v=y3LUlag7W1s
Abnormal Respiration and Oxygen
Abnormal respiration patters are described in healthcare contexts using some technical terminology. When communicating with other members of the care team it will be helpful for NAs to know some key terms about breathing[8].
- Apnea: not breathing, usually for a short period of time. Many people have sleep apnea, which means they temporarily stop breathing at times when they are asleep.
- Tachypnea: breathing abnormally fast
- Bradypnea: breathing abnormally slowly
- Hypoventilation: not taking in enough oxygen or removing enough carbon dioxide
- Hyperventilation: breathing very quickly and taking in too much oxygen
- Dyspnea: difficulty breathing
- Orthopnea: shortness of breath that only occurs when the person is laying down
EMTPrep. (2019, November 18). Hypoventilation and Hyperventilation – EMTprep.com [Video]. Youtube. https://www.youtube.com/watch?v=aVyAWjaGT8Q
Hypoxia
Hypoxia is the term for low oxygen levels. The symptoms of hypoxia occur across physical and behavioral systems because the entire human organism relies on oxygen. Symptoms of hypoxia include:
- restlessness
- disorientation
- confusion
- anxiety
- agitation
- fatigue
- changes in personality
- dyspnea
- orthopnea
- skin discoloration
- poor focus and concentration
- increased pulse
If any of these symptoms are observed, particularly when accompanied by other symptoms on the list, should alert the nurse.
Respiratory illness
Diseases that affect the respiratory system come in many different forms. These diseases can be acute or chronic; an acute disease is one that comes on somewhat quickly and has a relatively short duration, while a chronic disease lasts a long time and may be a lifelong condition.
While the goal of treatment is almost always to return a person to their normal functioning, approaches to treatment and the extent to which a respiratory illness impacts a person’s lifestyle may depend in part on whether the illness is acute or chronic. Sometimes managing symptoms is the only realistic care goal.
Chronic Obstructive Pulmonary Disease (COPD)
Chronic obstructive pulmonary disease (COPD) is a disease that gets worse over time that results in dyspnea due to obstructed airways. There is no cure for COPD, and if patients were smoking at the point of diagnosis then they must stop immediately[9]. Treatment can be helpful in hindering the disease’s progression, even though a return to full respiratory functioning is highly improbable. Chronic bronchitis and emphysema are the two illnesses grouped under COPD.
Chronic bronchitis occurs when the bronchial tubes become inflamed repeatedly and for long periods of time, and is caused by general air pollution, pollution in one’s environment (such as secondhand smoke), and cigarette smoking.
The bronchial tubes branch from the throat into the lungs and help to facilitate the gas transfer between the lungs and the environment; bronchial inflammation can result in difficulty breathing and chest pain. The scarring and long-term inflammation of the bronchial tubes leads to a persistent cough. Eventually the lung tissue also scars and becomes prone to irritation and infection.
Chronic bronchitis and cigarette smoking lead to emphysema, a disease where the air-sacs in the lungs, called alveoli, become damaged and break. Symptoms of emphysema are a persistent cough and dyspnea. Medications, oxygen, and respiratory therapy may be prescribed to slow the disease and make the person more comfortable.
When treating a person with COPD, always practice meticulous infection control practices, and follow the care plan closely concerning medications and oxygen delivery. It is also important to extend patience and understanding to residents’ feelings of anger, fatigue, anxiety, and frustration over their difficulty breathing and respiratory problems.
Pneumonia
Pneumonia is a respiratory illness caused by lung inflammation, and has many different causes. Depending on the cause, pneumonia may be communicable. The alveoli fill with fluid and lung tissue becomes inflamed, leading to difficulty breathing and an aggressive wet cough.
Pneumonia can be bacterial, viral, fungal, or in response to a pollutant; anything that causes the lungs to inflame and fill with fluid could be a potential cause of pneumonia. People at high-risk for developing pneumonia are the very young and elderly, habitual smokers, people who have had a stroke, people who are immobile or on bed rest, people with another respiratory illness, people who receive tube-feedings, and people who must use a ventilator.
Tuberculosis
Tuberculosis (TB) is a bacterial infection usually of the lungs, but can impact other areas of the body as well. Symptoms of TB include extensive coughing, dyspnea and chest pain, coughing up blood, fever, chills, and sweats, and exhaustion.
TB is airborne, which means it is spread through droplets of moisture and mucus expelled into the air through an infected person’s speaking, coughing, laughing, singing, etc.
A person is less likely to spread (or contract) TB in spaces with excellent ventilation and air circulation, and in a spaces where people wear PPE like masks and respirators.

Any tissues that comes into contact with mucus should be flushed or placed in a biohazard bag and re moved.
Caring for persons with respiratory illness
NAs can assist residents with respiratory illnesses by positioning them upright and making sure their body stays aligned. NAs may also position a person so they are bent over a table with a pillow on it; this position can take some of the weight off their chest and may partially alleviate dyspnea.
Some resident will need exercises including deep breathing and forceful coughing to help open their airways and slow the weakening of their chest muscles. Deep breathing and coughing exercises may be included in a person’s care plan to mitigate respiratory illnesses; always closely follow the person’s care plan.
Deep breathing
A deep breathing exercise involves taking a deep breath, holding it in for 3 – 5 seconds, and then exhaling as long as possible. A coughing exercise may follow a deep breathing exercise, and involves the resident holding a pillow or blanket tightly against their abdomen, taking a deep breath, and coughing as hard as they can. Have tissues and a basin ready to catch anything that is coughed up. Always check the care plan for details on the type of exercises and number of repetitions to use.
An incentive spirometer is a device used to dictate deep and slow breathing exercises, usually following surgery. NAs should prompt people to use the incentive spectrometer as prescribed in their care plan; however if the person is resistant or refuses the NA should not push the matter and should instead report it to the nurse instead.
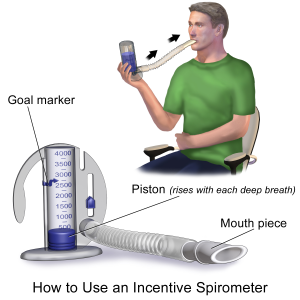
Image by BruceBlaus is licensed under CC BY-SA 4.0.
NAs should clean the mouthpiece of the spirometer device prior to use. The person should close their mouth around the mouthpiece and inhale slowly and deeply while trying to keep the indicator at the proper level. They can then exhale slowly. The number of repetitions and frequency of incentive spirometer exercises will be detailed in the care plan.
Oxygen delivery
Oxygen is totally essential to every part of the human body. Some people may require oxygen therapy, where oxygen is delivered directly to their lungs using mechanical assistance. A person may need additional oxygen delivery after a surgery, due to a respiratory illness, or any illness that impacts the person’s oxygen levels[10].
Some require additional oxygen temporarily or at different points throughout the day and night, while others may need to be connected to an oxygen device at all times.
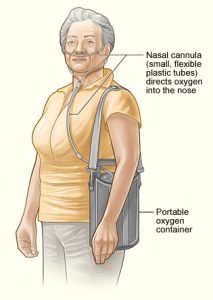
Oxygen is usually delivered either through a nasal cannula or by a face mask. A nasal cannula is a two-pronged device attached to a tube, where the prongs are inserted into the wearer’s nostrils. The cannula’s tubing is attached to the source of additional oxygen. Nasal cannulas are common in long-term care contexts.
Face masks fit over the nose, mouth, and chin of the wearer, are held there by a band that stretches around the wearer’s head above the ears, and are connected to an oxygen source by tubing similar to that used with a nasal cannula. Face mask oxygen delivery is less convenient and less comfortable than using a nasal cannula because it irritates the skin and prevents any talking, eating, and drinking.
Delivery systems
Additional oxygen may come from a wall outlet in the facility, from a tank of compressed oxygen, from an oxygen concentrator, or from a tank of liquid oxygen. 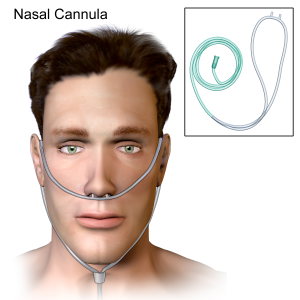
When the oxygen comes from the wall outlet, the cannula or mask’s tubing will simply hook into the designated spot on the wall in their room. If they are using a tank of compressed gaseous or liquid oxygen then the tank will likely be on a cart.
Oxygen concentrators are devices that gather oxygen from the surrounding air and deliver it to the recipient in a concentrated form; they come in various shapes, sizes, and levels of portability. Oxygen concentrators usually plug into electrical outlets.
BruceBlaus, CC BY-SA 4.0
National Heart Lung and Blood Institute (NIH), CC 1.0
Oxygen Safety and Comfort
Oxygen safety is paramount. Compressed and concentrated oxygen is highly flammable. Anything that could possibly cause a spark becomes an extreme fire hazard around an oxygen delivery system; no unnecessary electrical devices or wool linens around an oxygen system, nor anything that could cause a spark.
- It should go without saying, but nobody should ever smoke anywhere near an oxygen delivery system. Open flames must be kept far away from compressed oxygen. NAs should post “oxygen in use” signs on the doors and over the bed of residents using oxygen therapy. NAs should make a point of knowing where all facility fire extinguishers and alarms are located.

- Oxygen tanks must be well secured in their holders to prevent damage, oxygen leaks, and explosions. They must always be kept upright and in the proper holder. Oxygen concentrators should be used in a well-ventilated space with adequate air circulation.
- Never use petroleum-based products for a person’s skin care when they are on oxygen. NAs should use water-based lubricants and skin care products that do not pose a fire safety risk.
- NAs should observe the oxygen delivery tubing to make sure it is clean and free of kinks, and changed in accordance with facility policy. Image by Nesdon Booth (CCBY3.0)
- NAs should keep a close eye on the oxygen delivery system’s measurements: is the oxygen flow rate remaining at the level prescribed in the person’s care plan? Are the oxygen levels adequate, or does the person’s oxygen tank need to be replaced.
VITAS Healthcare. (2017, November 20). Demonstrations: The Dangers of Oxygen [Video]. Youtube. https://www.youtube.com/watch?v=LrfHnKtKvws
NAs should make a point of providing emotional support to persons on oxygen. Requiring an oxygen delivery system can be a jarring experience; they are uncomfortable, may be difficult to use and disruptive to a person’s routines, and can come with feelings of claustrophobia and loss of control. NAs should provide a listening ear, and encourage the person to continue with the activities they can healthily maintain so their psycho-social needs to do not go unmet.
Reporting and Recording
Report any adverse side-effects or indications of problems with patients using oxygen, including:
- sore, crusty, or reddened areas on the person’s skin
- discoloration in the person’s skin or eyes
- changes in vital signs
- complaints of pain and tightness
- dyspnea
Artificial airways
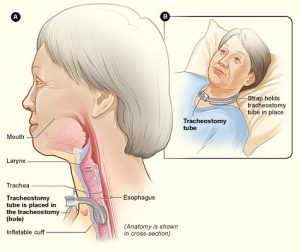
A person may need an artificial airway to ensure that their airways are kept open so the lungs can continue to take in new oxygen and expel carbon dioxide. Without an open airway the lungs cannot function, and the person will not have enough oxygen to live.
Artificial airways are necessary when the person’s airways would otherwise be obstructed due to illness, injury, or surgery. An artificial airway is created when a doctor or nurse inserts a tube, through a process known as intubation, into the person’s windpipe (trachea). The tube may be inserted through the person’s mouth or nose, or through a surgically created opening in the neck. There are a few different kinds of artificial airways[11].
An oropharyngeal airway is a relatively short, curved plastic tube inserted through the person’s mouth that prevents their tongue from blocking their airway.
An endotracheal airway is inserted through the person’s mouth or nose, and extends into their trachea and sits between their vocal cords.
A tracheostomy is a surgically created stoma in the neck that leads into the trachea. A tracheostomy tube delivers oxygen directly into the trachea. People with tracheostomies will need attentive, sanitary care.
- Caring for a tracheostomy includes maintaining meticulous infection control measures by cleaning the area around the stoma (opening), helping the nurse with changing dressings, and assisting with cleaning the tracheostomy tubing. If the NA notices any gurgling or otherwise abnormal noises coming from the device when the person breathes, they should tell the nurse since the tubing may need to be cleaned.
- Perform oral care every two hours as directed in the care plan. Patients with tracheostomies are at high risk for aspiration, so oral care may need to be performed with specific tools meant for people using artificial airways.
-
NAs should not change anything about a tracheostomy device. Do not to move or jostle any tubing while performing oral and skin care.
- Tracheostomies are cleaned using a process called suctioning. Suctioning involves the use of a pump to remove all secretions from the person’s airway, and may need to be done regularly. NAs cannot perform the suctioning procedure, it must be done by a nurse or a respiratory therapist. If a person with a tracheostomy shows signs of respiratory distress such as noises, shortness of breath, or pain then they may need suctioning.
- NAs should be as supportive as possible when a person needs an artificial airway, particularly during moments of acute discomfort. When a person is having extreme difficulty breathing, maintaining conversation and light touch can be comforting.
National Heart Lung and Blood Institute (NIH), CC 1.0
Caring for artificial airways
When caring for somebody with an artificial airway, NAs should regularly closely inspect the tubing and any adhesives that keep tubing in place. If the tubing falls out or comes undone, remain with the person and alert the nurse using the person’s call light.
Artificial airways are uncomfortable. Always practice empathetic communication. Some people using artificial airways cannot speak, so the NA will have to devise alternative means of communication through writing, typing, or gestures.
If the NA observes any signs of abnormal respiration, discoloration in the skin or eyes, secretions in tubing, drainage from surgical sites, or emotional distress, they should alert the nurse.
Mechanical ventilators & chest tubes
A person who cannot breathe on their own may require the assistance of a mechanical ventilator to breathe for them by automatically moving air into and out of the lungs. Ventilators supply a person’s body with oxygen through an artificial airway; because the air bypasses the larynx and vocal cords, a person using a mechanical ventilator will be unable to speak. NAs should be a frequent and calming presence to a person on a ventilator by checking in with them, spending extra time with them if possible, and devising modes of communication to use when the person cannot speak.

NAs should pay close attention to a person on a ventilator, and always make sure that their call light is easily within reach.
If there are any alarms or irregular beeping coming from the mechanical ventilator, notify the nurse immediately. Notify the nurse if a person on a ventilator is exhibiting any signs of respiratory distress, or pain and discomfort.
Practice careful infection control with people who are using ventilators; HAIs are common results of ventilator use in facilities.
NAs will not hook or unhook anybody to or from a mechanical ventilator. The NA’s primary role will be to closely observe the ventilator’s tubing and connections to make sure everything is smooth and free of blocks or kinks, and to provide oral care often and as directed. NAs should work with the person to find effective ways of communicating when they are unable to speak.
Image by BreathDriver, CC BY-SA 4.0
A person may require chest tubes in between layers of lung tissue to help drain air, blood, or other fluids. The tube is attached to a drainage system which allows for the removal of gas or fluids.
NAs must be careful and aware of all tubing and tubing connections, and try to prevent kinks from forming. The system must be completely airtight.
The drainage collection system must be kept below the person’s chest at all times.
The NA should notify the nurse immediately with any changes in the condition of the ventilation system or the patient. Indications of respiratory distress, disconnected or malfunctioning tubing, and coughing up blood must be urgently addressed.
The Nursing Assistant’s Role
NAs have a specific and important set of responsibilities when caring for respiratory patients using oxygen, artificial airways, and chest tubes. While NAs do not insert or connect oxygen, artificial airways, or chest tubes, they perform vital tasks in their observation, and in the care of the people who need them.

- NAs should regularly check to make sure that the oxygen flow is set to the correct amount. Always ask or check the care plan if unsure about a person’s prescribed oxygen treatment. If the oxygen flow is incorrect, tell the nurse immediately.
- A person’s mouth, nose, and skin can develop sores and irritation when using respiratory equipment. Maintaining good oral and skin care can help make a person’s experience less uncomfortable, and will help prevent infections. Maintain communication throughout care tasks even when the person is unconscious and unresponsive.
- Follow the care plan instructions for deep breathing and coughing exercises, and incentive spirometer use. Remain positive and encouraging during these exercises, and exercise patience and empathy when the person expresses frustration.
- Reposition people frequently in accordance with the care plan and instructions from the nurse.
- Alert the nurse immediately if observing any disconnections in the oxygen equipment, any changes in the amount or quality of the drainage, changes in the condition of the device or the person, and any signs and symptoms of hypoxia or respiratory distress.
- Observe and chart carefully and thoroughly.
Key Takeaways
- Vital signs are measurements of some mechanisms part of a body’s basic functional processes. Vital signs include temperature, pulse, respiration, and blood pressure. It is essential that NAs take vital measurements accurately, and alert the nurse if a resident’s vital signs are abnormal.
- Always obtain vital signs properly and respectfully. Chart vitals right after taking them so they are remembered correctly. If temperature, pulse, blood pressure, or respirations are abnormal, they may clue the care team into an ongoing problem or an active medical emergency.
- Hypertension and hypotension are common cardiovascular disorders. While both are dangerous, hypertension can be deadly, cause heart attacks, and points to severe cardiac diseases. Chronic obstructive pulmonary disease (COPD), pneumonia, and tuberculosis are some common respiratory diseases. COPD is an incurable respiratory disease that progresses as alveoli and lung tissue scar and engage in excessive mucus production.
- Some patients may require additional oxygen using an oxygen supply or a mechanical ventilator. When using an oxygen supply, the oxygen will either be delivered using a nasal cannula or a face mask. NAs should not hook up oxygen, unhook oxygen, or change any of the levels on an oxygen supply device. When caring for someone using additional oxygen, make sure that they are comfortable, the tubing is free of kinks that could block flow, and the oxygen is flowing at the rate prescribed in the care plan. Always practice oxygen-specific fire safety, and do not use items that may produce a spark.
Comprehension Questions
1) The normal temperature range for a human is considered to be _____ degrees Fahrenheit, though it varies depending on factors like age, activity level, and illness.
a.97.6 – 99.6
b. 98 – 99.5
c. 97 – 99
d. 96.6 – 98.6
2) Please list the four vital signs, and describe what each of them mean.
3) The systole is ________ , while the diastole is __________ .
a. the top number on a blood pressure reading; the bottom number on a blood pressure reading
b. the atria; the ventricles
c. the motion of the heart as it contracts; the motion of the heart as it refills with blood
d. “dub”; “lub”
4) Respiration is _________ ; the body takes in ______ to distribute throughout the body, and removes _______ .
a. the exchange of gas between a person and their environment; oxygen; carbon
b. the inhalation of fluids during eating and drinking; food or fluid; air
c. the exchange of gas between a person and their environment; air; oxygen
d. the exchange of gas between a ventilator and a person; carbon; oxygen
5) Respond to the following sentences with T (true) or F (false).
____ Aging impacts the circulatory system as hemoglobin decreases and blood vessels harden.
____ Symptoms of hypoxia include oxygen saturation, restlessness, and high energy levels.
____ Some respiratory illnesses cannot be cured. When an illness cannot be cured and lasts a long time it is acute.
____ Hyperventilation includes an excess of oxygen.
____ Someone experiencing hypoxia may act differently, and not seem like themselves.
6) How does someone use an incentive spirometer?
a. By exhaling forcefully into the mouthpiece to get the piston as high as possible
b. By shaking it up and down while inhaling and exhaling slowly
c. By inhaling slowly and trying to keep the piston at the appropriate level
d. By inhaling deeply and blowing back into it again
7) Which of the following should nursing assistants do for someone receiving oxygen therapy? Select any that apply.
a. Adjust the oxygen levels to the prescribed levels in the care plan
b. Remove nasal cannula tubing for cleaning
c. Provide careful skincare around the cannula or mask area
d. Carefully observe the resident for signs of difficulty breathing, and observe but do not change oxygen settings.
8) What is a tracheostomy?
a. An opening through which mucus and secretions can be removed from the lungs
b. A stoma in the neck that allows somebody with mouth sores to speak
c. An opening in the neck that allows oxygen to be pushed directly into the trachea
d. An opening in the neck that removes drainage from the vocal cords
9) Please list at least three adverse side-effects of oxygen use nursing assistants should report to the nurse and record in the resident’s chart.
10) Respond to the following sentences with T (true) or F (false).
____ Oxygen may come from a wall outlet, a portable oxygen tank, or a device called an oxygen compressor.
____ Smoking near oxygen is acceptable as long as you blow the smoke away from the tank.
____ Residents receive oxygen through a nasal cannula, a face mask, or in liquid form.
____ Post an “oxygen in use” sign outside of resident’s doors when they use oxygen so that the rest of the healthcare team is aware of the fire hazard.
____ When tracheostomy tubing becomes disconnected, NAs should hook it up again as quickly as possible as long as they have been trained.
11) Think back to the nursing process (assess, diagnose, plan, implement, evaluate/assess). What goes into each step of the nursing process, and what role do vitals measurement play in each step?
12) How might oxygen use impact someone’s psychosocial needs and wellbeing? How should nursing assistants respond to a person for whom oxygen use is negatively impacting their emotional and social wellbeing?
- Vital Sign Measurement Across the Lifespan - 2nd Canadian Edition by Jennifer L. Lapum; Margaret Verkuyl; Wendy Garcia; Oona St-Amant; and Andy Tan is licensed under a Creative Commons Attribution 4.0 International License, except where otherwise noted. ↵
- RegisteredNurseRN. How to take temperature in 6 different ways. https://www.registerednursern.com/take-temperature-6-different-ways/ ↵
- May Clinic Staff. How to take your pulse. https://www.mayoclinic.org/how-to-take-pulse/art-20482581 ↵
- Cleveland Clinic. Apical Pulse. https://my.clevelandclinic.org/health/articles/23346-apical-pulse ↵
- Sorrentino, S. A., & Remmert, L. N. (2019). Mosby's essentials for nursing assistants (6th ed.). Elsevier. ↵
- Nursing Assistant, Chapter 7 by Chippewa Valley Technical College is licensed under a Creative Commons Attribution 4.0 International License, except where otherwise noted. ↵
- Dugan, D. (2020). Nursing assisting: A foundation in caregiving (5th ed.), Chapter 20. Hartman. ↵
- Sorrentino, S. A., & Remmert, L. N. (2019). Mosby's essentials for nursing assistants (6th ed.), Chapter 30. Elsevier. ↵
- World Health Organization. Common Respiratory Diseases. https://www.who.int/health-topics/chronic-respiratory-diseases#tab=tab_3 ↵
- American Lung Association. Oxygen Therapy. https://www.lung.org/lung-health-diseases/lung-procedures-and-tests/oxygen-therapy ↵
- NetCE. (2020, November 1). Respiratory Care: Artificial Airways, Mechanical Ventilation, and Chest Tubes. https://www.netce.com/coursecontent.php?courseid=2094 ↵
How much heat is being generated by a person's body
The number of times a person's heart beats per minute
Breathing, or number of breaths
The amount of force exerted by blood against the arterial and vascular walls
The heart's contracting and pushing blood throughout the body
The heart relaxing and filling with blood again
Low blood pressure
Low blood pressure brought on by moving from a sitting to a standing position
High blood pressure
blockage of the blood vessel
Insufficient blood supply to a given area
A tool used to take blood pressure. It consists of an arm band, a pressure gauge, and sometimes a handpump.
absence of breathing
difficulty breathing
Small blood vessels that cover the body and distribute blood to tissue
breathing abnormally or unhealthily fast
breathing abnormally slowly
Not taking in enough oxygen, or removing enough carbon dioxide. There is too much carbon dioxide in the blood.
Breathing too quickly and taking in too much oxygen
Low oxygen levels
Breathlessness while sitting, which is relieved when standing
A disease that comes on quickly and lasts a relatively short duration
A disease that lasts a long time, and may be a lifelong condition
A progressive disease that causes difficulty breathing due to obstructed airways. Airways may be obstructed by factors such as inflammation and respiratory breakdown.
A respiratory illness caused by lung inflammation and the alveoli filling with fluid
Devices used to keep a person's airways open and unobstructed
Short plastic tube that prevents a tongue from blocking an airway
A tube that is inserted into a person's mouth and sits between their vocal chords
Surgically created opening in the neck that allows air to enter the trachea directly
A machine that moves air into and out of the lungs for people who cannot do it themselves
