7 Module 7 – Personal Care
Personal Care of the Patient
Learning Objectives
- Demonstrate understanding of the need for good hygiene
- Demonstrate the ability to perform hygiene tasks
- Demonstrate understanding of the safety precautions related to activities of daily living
- Demonstrate understanding of the importance of excellent skin care
Personal care refers to a person’s hygiene, or the steps someone takes to keep themselves clean and healthy. Some examples of hygiene practices are showering and brushing one’s teeth.
Personal care also refers to grooming, such as trimming one’s fingernails and toenails or brushing one’s hair. Personal care tasks are part of what make up a person’s activities of daily living (ADLs), and NAs will assist people with personal care ADLs every day.
Many people enjoy their personal care routines throughout their lives; perhaps it was part of their sense of independence, or moments they had to themselves. Requiring assistance with personal care due to old age or a medical intervention can come with feelings of loss of independence, sadness, or frustration.
To make these moments easier, NAs can try and make time spent on personal care tasks fun. Some ways to do this are to cultivate a positive relationship with the person by telling a happy or funny story, or asking the resident questions about themselves with genuine curiosity. Talk with them while providing personal care.
Hygiene Matters
Hygiene is a topic that relates to the Big Three. Residents have a right to good care, and if they are not having their hygiene needs met then their quality of life will suffer. Good hygiene is also an important part of infection control and prevention because it cleanses the body and mouth of potentially harmful pathogens.

Good hygiene has many health benefits. It cleanses the outside of the body, dirt, and other irritants. Maintaining good hygiene also helps to prevent unpleasant odors from someone’s body and breath. including sweat, eliminations.
Hygiene routines
Over time a person’s illness or aging process can get in the way of performing personal care independently. NAs must recognize the necessity of attentive hygiene to a person’s quality of life and, in addition to meeting their basic hygiene needs, work to make time spent addressing hygiene needs dignified, personable, and even fun.
Remember that residents have a right to dignity and privacy that is especially important during hygiene care.
![]()
hygiene by Andrejs Kirma (CCBY3.0)
People have different relationships to hygiene, and may usually follow a personalized hygiene routine when not in a facility. Cultural background can impact how often a person washes and how they wash.
Hygiene routines are also influenced by factors such as personal choice and preference. NAs should try and meet a person’s personal hygiene preferences as long as the NA also closely follows the care plan and meets the person’s hygiene needs as they have been determined by the nursing process.
For example, if the nurse determines that a person must have their teeth brushed twice per day with a prescription toothpaste then a person’s wish to use a particular brand of store-bought toothpaste, should be explained to that person as inconducive to their health and recovery; however, the person’s right to choice and to be an agent of their own care needs to be respected and encouraged whenever possible.
Hygiene needs
Hygiene needs depend on someone’s condition; perhaps they require a prescription toothpaste, or you have to consider their bed sores during bathing, or perhaps they need a medicated lotion, or can only be given partial baths due to weakness.
Each person’s hygiene needs will be different. The important thing for the NA is to always follow the care plan.
Nursing assistants should always observe the resident closely to assess how care is going. If you notice anything during the time spent providing hygiene care, whether it is a change in a person’s skin condition, mouth sores, or orientation, chart it and let the nurse know in case something in the person’s care plan needs to be adjusted.
When does personal care occur?
Personal care will be given three times per day, and whenever the resident requests it. Different kinds of care will be required at different times of the day; the schedule of care, in addition to necessary care tasks, will be detailed in the person’s care plan. NAs should always check with the care plan or check with a nurse if they are unsure about something in a person’s hygiene schedule.
- Morning care begins with gently waking someone and continues after breakfast. Such care may involve brushing teeth or dentures, shaving, using the toilet or commode, and bathing or showering depending on the person’s preferred schedule. Morning care will also involve helping the person dress for the day.
- Afternoon care is done between lunch and the evening meal. Some residents may prefer to shower in the afternoons, while others may not need bathing or dental care but may want their fingernails trimmed. NAs must remember to offer the restroom to people often. Some people will also want to brush their teeth or care for their dentures after their midday meal.
- Evening care involves assisting residents with their bathroom needs, dental care, bathing, and with putting on pajamas. Evening is also the time to care for the resident’s space by changing soiled linens and decluttering.
Assist with hygiene whenever the person requires it. Residents have a right to comfort and to safety, and a person is neither comfortable nor safe when their hygiene needs go unmet.
Resident Rights
It is important that NAs work to provide care tasks in a way that affords the person dignity and respect. They can do this by encouraging as much independence as possible; a person should be prompted to perform whatever care tasks they can perform on their own.
Be patient – even if somebody takes a long time to do something unassisted, if they can and they want to then you should be patient and encouraging for as long as the process takes. Briskness and frustration do not make someone feel cared for.
Always plan for privacy. When assisting somebody with personal care tasks, the NA should ensure that the person has privacy by closing the door to their room and putting the privacy screen in place.
Hygiene care is closely related to both Resident Rights and Infection Control. Write about the connection between hygiene care and the Big Three – why is hygiene important for good Infection Control? What elements of Resident Rights should NAs keep in mind when giving hygiene care? Write for 5 minutes and share your response with a friend or classmate.
Assisting with hygiene
Bathing
Everyone needs bathing. Bathing is important to our health, and helps people feel comfortable and refreshed. The benefits of bathing include:
- Removing microbes, dead skin, sweat, and oils
- Cleansing the mucus membranes in the genital and anal areas.
- Stimulating circulation
- Provides and opportunity for some basic range of motion exercises
Many people enjoy bathing, and will find their hygiene routines refreshing and relaxing. In addition to the medical benefits of bathing, there psychosocial benefits as well.
Bathing is a great time to talk with the resident because it is an extended period of time with individual attention. This could be a casual conversation where you continue to foster a rapport, or it could be an opportunity for a resident to discuss a problem they have been having.
Bathing presents NAs with an opportunity to closely observe the resident’s behavior, orientation, mood, and the parts of their body that are usually covered with clothing. Always observe closely, and report and record anything relevant.
Types of baths
The four basic types of baths are a partial bath, a shower, a tub bath, and a complete bed bath.
When deciding what kind of bath to give a resident, always check the care plan, determine the person’s needs, and take their preferences into account. The orders from the doctor or nurse are prioritized over the preferences of the patient in this case; for example, if the doctor ordered full bed rest, then the person cannot get up for a shower, even when they would prefer one to a partial bath. However, the person’s preferences should be accommodated whenever it is possible and consistent with their care plan[1].
- Partial bath: Partial baths can be given while the person remains in bed. A partial bath involves washing the person’s face, underarms, hands, and the genital and anal area (the perineal area), and any area that appears dirty or smelly. Partial baths are useful for people who can’t get up or don’t want to get up for a full bath or shower, have sensitive skin, or who want to freshen up.
- Shower: Residents should shower if they can safely stand for the duration of the shower or are comfortable sitting in a shower chair. Residents who are fatigued or prone to dizziness should avoid showers.
- Tub bath: Tub baths take place in bathtubs. Tub baths are intended for residents who are capable of transferring into and out of a bathtub, and who prefer a bath to a shower.
- Complete bed bath: A complete bed bath is intended for people who cannot get out of bed but who still require a full bath, rather than a partial bath.
The order of bathing
The order of bathing is important, and is part of good infection control practices. The order of a bath is intended to keep potentially harmful microorganisms from spreading to different parts of the body where they could cause infection.
When bathing a resident, the order of the bath must go as follows:
1. Eyes
2. Face
3. Ears
4. Neck
5. Arms and hands
6. Chest and abdomen
7. Legs and feet
8. Back
9. Perineal (genital and anal) area
10. Buttocks
This order is the same for a full bath, shower, bed bath, and partial bath.
Watch the video below for a demonstration on how to give a full bed bath.
Chippewa Valley Technical College. (2022, December). Full Bed Bath. [Video]. YouTube. Video licensed under CC-BY-4.0
Safety
Bathing safety is absolutely necessary when assisting with personal care.
The first step in providing a safe bath, of any kind to prepare well. Have everything you need within arm’s reach, and ask for any help that they think might be necessary during the bathing process.
The importance of prepping one’s supplies comes from the need to remain with the person during the entire bathing process – never leave someone alone when they are in the bath or shower.
When preparing a bath or shower, NAs must be conscious of a resident’s diminished sensitivity to temperature sensations and the increased fragility of the resident’s skin. Burns and chilling from water are dangerous if NAs are not conscientious when preparing a bath or shower. The water in a bath or shower should not exceed 105 degrees Fahrenheit.

Perineal care
Perineal care, or the cleaning of the anal and genital region, is completed every time a person bathes or whenever waste or urine is present. Perineal care is extremely important for infection control and promotes comfort by eliminating odors and skin irritants.

Perineal care is especially important for people who have urinary catheters, have had perineal surgery, are actively menstruating, are incontinent of urine or feces, and are uncircumcised (the foreskin of the penis was not removed). All of these factors make somebody more susceptible to perineal infections and concentrations of microbes.
Patients and residents will perform their own perineal care if they are physically able to; some obstacles to a person doing their own perineal care might include lack of mobility and flexibility or an order for complete bed rest.
When providing perineal care, always clearly communicate exactly what you are about to do before doing it. The goal is to always have the person receiving care know what is about to happen and be able to prepare themselves for it, and to have received that information in a way that they understand and helps them stay comfortable and calm.
When providing perineal care, NAs must always follow the Standard Precautions (wear gloves!), the Bloodborne Pathogen Standard, and the protocols of medical asepsis.
How to provide perineal care
Use warm water, as opposed to hot water, and soap in small amounts. The process includes items such as a washcloth or towelette and an emesis basin; NAs should always follow facility policy on the items used to perform perineal care.
Always move “front to back” when performing perineal care. For a person with a vagina, this will involve gently separating the labia majora, which are the external folds of skin that protect the vaginal and urinary openings, and wiping front to back on either side. Use a different section of the washcloth when moving to different parts of the perineal area.
After washing the genital region, clean the perineum (the area between the genitals and anus) before rinsing the perineal region with a clean washcloth. Pat the area dry from front to back, and then help the person into some clean undergarments.
Chippewa Valley Technical College. (2022, December). Perineal Care – Female. [Video]. YouTube. Video licensed under CC-BY-4.0
When cleaning the perineal area of someone with a penis, keep using the front-to-back motion. If the person is uncircumcised, gently pull the foreskin back and clean the area under the foreskin. The penis should be cleaned in a circular motion moving front to back, with a new section of the washcloth used for each region of the perineal area.
After rinsing with a non-soapy washcloth, return the foreskin to its normal position. Once the penis has been washed and dried, the NA can move on to clean the groin. Finally, using a fresh washcloth, the NA can clean the buttocks and anal area and pat dry.
Chippewa Valley Technical College. (2022, December). Perineal Care – male. [Video]. YouTube. Video licensed under CC-BY-4.0
Report & Record
NAs should always report and record whenever hygiene care of any kind is given. If care is not properly recorded, the rest of the care staff will assume that care was not given. In addition to the importance of recording that personal care took place, use personal care time to make observations about the person’s condition.
When observing during personal care, it is important to look for any signs of bleeding, skin breakdown, any discharge from the vagina or urinary tract, any foul or unusual odors, or any changes (positive or negative) in the person’s condition since the last time observations were recorded.
Recording all personal care and any observations made is necessary for providing good care. It is also necessary from a legal perspective, both because records maintenance is a requirement for facilities, and because failing to record care could lead to legal problems resulting from medical negligence. Both the person receiving care and every other member of the care team rely on NAs to report and record thoroughly.
Back rubs
One way that NAs can take some time to closely observe the condition of a person’s skin while helping them feel comfortable and relaxed is to give them a backrub.
To perform a back massage or a back rub, first position the person on their side or on their stomach. Next, warm the lotion between one’s hands or by running the bag or bottle under warm water, and apply lotion to one’s own hands.
Begin moving hands in wide circular motions starting at the base of the spine and reaching up to the person’s shoulders without lifting them off of the person’s back; the massager should use firm strokes on the muscle tissue on either side of the spine, and gentle pressure on bony areas such as the spine and hip bones. The massage should last for between three and five minutes, and communication should continue throughout.
Back massages are a good opportunity for NAs to take note of changes to a person’s skin condition. Prior to beginning the massage, take a moment to closely examine the person’s skin for signs of breakdown.
Chippewa Valley Technical College. (2022, December). Back rub. [Video]. YouTube. Video licensed under CC-BY-4.0
Shampooing
Providing personal care will also involve shampooing residents. Shampooing may be done during the person’s shower or tub bath, at the sink, on a stretcher, or while the person is in bed.
In bed
- Make sure that all supplies are within easy reach.
- Water temperature must not exceed 105 degrees F.
- A shampoo tray will be placed beneath the person’s head to prevent water spilling on the linens – the pillows should be removed from the bed.
- The basin of water should then be placed beneath the person’s hair. Use a pitcher to get the person’s hair wet before massaging their scalp with shampoo, rinsing thoroughly, and helping the person dry their hair by wrapping a towel around their head.
At the sink
- The person will place their head against the padded headrest. If there is no padded area, place a folded towel on the edge of the basing to provide some comfort.
- It is important that the person’s neck is not placed at an angle – they need to maintain good neck alignment throughout the shampooing process for comfort and spinal health.
- Make sure the person is comfortable and that they are not getting soap or water in their eyes.
On a stretcher
- Set the stretcher to the same height as the sink and place it against the basin.
- Make sure the wheels are locked.
- Side rails of the stretcher should be raised during shampooing.
- Place a towel under the person’s head as their hair dries.
Tub or shower
- Make sure the water is at a suitable temperature before allowing the person to enter the shower or bath; it is a good idea to let them test it.
- If using a shower chair, make sure the wheels to the chair are locked. If using a tub, transfer the person into the tub and then fill the rub roughly halfway.
- Never leave someone alone during a shower or a bath.
-
To promote independence and dignity, the person taking the shower or bath should be encouraged to perform as much of it as they can themselves.
- Once the person is finished, help them dry off by patting them with a towel. Make sure they are completely dry.
The person’s hair should be styled and dried as quickly as possible after washing. NAs should always check with the nurse before curling somebody’s hair. Many people, especially residents in long-term care facilities, will have their hair done by a beautician. Some facilities will even hire a beautician to come in regularly for the residents who want their hair done.
A note on hair and respect
Always ask the person how they want their hair interacted with. This is an aspect of basic respect and of cultural competency. Different hair behaves differently, and the last thing a NA wants to do is do something unhealthy, damaging, or unwanted to someone’s hair. Hair can be something with personal and cultural relevance, and having their hair done correctly while living in a facility may be one of the things that helps a person feel like themself. Always be conscious of the potential importance of hair to a person, and use hair care as an opportunity to make someone feel agential and respected.
Oral care and hygiene
Oral hygiene refers to the care of the mouth, gums, and teeth. NAs will provide oral care to residents at least twice per day, although possibly more. Any action taken to care for someone’s mouth area or dentures all falls under the umbrella of oral hygiene[2].
Oral hygiene is important for preventing bad breath, removing plaque, and preventing gum disease. Maintaining a healthy mouth is worthwhile for its own sake; it is uncomfortable and unpleasant to have mouth discomfort and pain.
Good oral hygiene can also help a person be more confident, can make eating a more pleasant experience and make food taste better, can improve one’s overall attitude and comfort. Since plaque buildup can result in clogged arteries and heart problems, good oral hygiene also makes somebody less susceptible to heart disease, strokes, and diabetes.
Performing oral care
When providing mouth care, always communicate with the resident throughout the whole process, practice Standard Precautions, and let the resident perform as much of their own care as possible to encourage feelings of autonomy and independence.
Teeth, gums, tongue
- To brush a resident’s teeth, gums, and tongue, always communicate with the resident throughout the process.
- After performing the opening procedure and prepping a work station, make sure the resident’s bed is angled to a comfortable upright position and that the bed wheels are locked.
- Cover the resident with a towel, then wet a soft-bristled toothbrush and prepare it with a dab of toothpaste.
- Clean the resident’s whole mouth, including teeth, tongue, and gums with short, gentle brushstrokes. Once finished have the resident rinse their mouth with water and spit into the emesis bin.
- Return mouth care supplies to their location, then empty, rinse, and dry the emesis bin and place it in “dirty” storage. Place used linen in the appropriate receptacle. Make sure the resident is comfortable before returning the bed to its lowest position.
Flossing
- Prepare the station by raising the bed to the appropriate height and gathering the materials. Always use the privacy curtain when providing personal care.
- Wrap either end of the floss around the index fingers of both hands and gently move the floss downward between the teeth in a back-and-forth motion, beginning with the teeth in the back of the person’s mouth. Adjust the floss every two teeth so that there are always working with a clean section of floss.
- Once flossing is completed, offer the resident a glass of water and a basin so they can rinse their mouth and spit.
- When done, the NA can discard the used floss and water, and properly clean and store all supplied. Return the bed to its lowest height setting, and perform the closing procedure.
- Make sure the resident is comfortable and give them the opportunity to converse about whatever they want to talk about, since conversation is rather difficult when one’s teeth are being flossed. Always observe the resident’s mouth closely and report any changes, abnormalities, or bleeding.
Denture care
Many older adults use dentures, or fabricated teeth. Dentures in come in a half set (a full row of teeth on the top or bottom), a full set, a partial plate or a bridge, which replaces sections of missing teeth.
Dentures need to be made according to detailed specifications, and are difficult to make. They are very expensive. Handle dentures, and dental appliances in general, with the utmost care.
If dentures become damaged or chipped then it will likely prevent the person that uses them from eating. If the NA damages a person’s dentures then the facility is legally responsible for their replacement.
- Always practice Standard Precautions when handling dentures by wearing gloves and any other necessary PPE. Never place dentures on a contaminated surface.
- Dentures are cleaned much like teeth are brushed, except they must be removed from their wearer’s mouth before they can be brushed. First the NA should line the sink with a towel, and then fill the sink with water so the dentures will not break if dropped.
- If the resident cannot remove their own dentures, NAs should use a gauze pad to firmly but gently grasp the dentures and pull to remove them.
- Rinse the dentures in cool water (never warm or hot) over the sink before brushing them; dentures can be more easily damaged when they are dry, which is also why they must be kept moist or wet.
- Use the brush to thoroughly clean the dentures with denture cleanser (check the care plan), and then rinse them under cool water again. When finished, put the dentures into their clean container with denture fluid or cool water and place it where it is stored. Give the resident an opportunity to rinse their mouth and spit.
- If the resident wants to wear their dentures all the time other than during cleaning, the NA can replace them in the resident’s mouth by applying some denture cream and pressing them firmly back into place. Finally, clean the brush and emesis basin and return them to their storage location.
Chippewa Valley Technical College. (2022, December). Denture care. [Video]. YouTube. Video licensed under CC-BY-4.0
Oral care for the unconscious
If someone is unconscious for long periods of time, they still need mouth care. Even if a resident is unconscious, always interact with them as if they were by communicating throughout the process and keeping face-to-face contact. Always practice Standard Precautions and adjust the bed to a comfortable head to provide mouth care.
- Turn the resident on their side, with a towel under their cheek and chin and an emesis bin close by, since the unconscious resident may drool or allow fluid to leak from their mouth.
- Keep the resident’s mouth open with a tongue compressor; using one’s fingers is dangerous for both the NA and the resident.
- NAs won’t brush an unconscious resident’s teeth. Instead, use a sponge swab to apply a cleaning solution to all parts of the person’s mouth. Squeeze the sponge swab in between replenishing it with the cleansing agent and applying it to the person’s mouth; any drippage or excess fluid could cause aspiration. Change out the swab regularly until the mouth is clean.
- Always check the care plan when preparing to care for unconscious residents. The care plan will determine which cleansing agent to use, and include any necessary information to keep in mind. Continue to communicate with an unconscious person as if they are awake; you do not know what they can hear.
Assisting with grooming
Grooming is distinct from hygiene, and is also an essential dimension of a person’s healthcare. Grooming includes:
- styling hair
- trimming fingernails
- dressing and changing clothes
- applying makeup and jewelry
Grooming has an impact on how a person feels about themself – it is part of multiple layers of Maslow’s hierarchy, and contributes to self-esteem and self-actualization. Assisting someone with grooming helps them meet their psycho-social needs.
Grooming is important for preventing infection and promoting comfort. Everybody has their own grooming routine and preferences. Some grooming habits are personal, while others are influenced by culture and context. The person should be encouraged to tend to their own grooming as much as possible, with basic assistance and the company of a NA.
Hair care
NAs should assist a resident with hair care whenever the resident wants. The care plan will include specific directions on how to care for a person’s hair.
The nursing process and care plan should reflect the person’s culture, their personal choices and preferences, the condition of their skin and scalp, their relevant health history, and their ability to perform self-care unassisted. All of these factors play an important role in determining how best to care for a resident’s hair.
Brushing and combing
Brushing and combing is a regular part of early morning and afternoon care, and should be provided whenever the resident wants it, and always before they receive visitors. NAs should encourage residents to perform as much of their haircare as possible, and assist them as they need it.
The person will choose how their hair is brushed, combed, and styled. NAs should never cut a person’s hair because it is matted or tangled; instead, check in with the nurse and the person about appropriate ways to manage hair care. Specific measures are required for brushing and combing curly, coarse, and dry hair. A person’s haircare routine and preferences will be included in their care plan.
Skin and scalp conditions
Skin and scalp conditions can impact a person’s quality of life. Carefully observe for skin conditions during hair care, and always remain composed and respectful not matter how someone’s head looks.
- Alopecia is a term meaning hair loss, and alopecia to different degrees is experienced by most people throughout aging in the form of balding or thinning. Other causes of alopecia include cancer treatments, skin diseases, stress, poor nutrition, pregnancy, side affects from drugs, and changes in hormones.
- Hirsutism is a term for an excessive or abnormally high level of body hair. Hirsutism occurs in men, women, and children due to heredity and high testosterone.
- Dandruff occurs when the scalp or eyebrow skin produces a lot of flakes; people with dandruff may require medicated shampoos to address the itching and flaking.
- Pediculosis is the medical term for infestation with head lice. Lice are nearly impossible to see with the naked eye. Lice are highly communicable and can travel through contact, clothing, furniture, towels and linens, or shared items like hats and combs.
- Symptoms of lice include complaints of tickling or movement in one’s hair, itching and skin irritation, sores on the head or body from scratching, or a rash.
- If you think someone may have pediculosis, alert the nurse right away and follow the care plan for treatment.
Shaving
People shave for comfort, mental wellbeing, and self-esteem. NAs will likely need to shave a person’s face, legs, and underarms at different intervals. NAs will use either an electric razor, a safety razor, or a disposable razor to shave a person.
- After performing the opening procedure, communicate with the resident while preparing the station with razors, shaving cream, a basin of warm water, and a sharps container. Before beginning to shave, the wet the person’s skin with warm water and then lather the area with shaving cream.
- While shaving, hold the person’s skin taut and shave in the direction of hair growth; if shaving a person’s face, this will involve shaving down the cheeks and up the neck. To shave the spaces just below and above the lips, have the person pull their lips into their mouth and over their teeth to keep the skin tight.
- The razor blades in facility settings will likely become dull before the shave is over, so multiple blades will needed; razors must be disposed of in the sharps bin when dull. NAs should always try to keep the razor blades fresh for a close, comfortable, and cut-free shave.
Some residents cannot use safety razors or disposable razors, especially if they have difficulty healing or are on drugs that inhibit blood clotting. For these residents, NAs will use an electric razor. Make sure the razor is clean before using, and never use an electric razor around water or oxygen.
People with mustaches and beards will need daily facial hair care. NAs should always ask the person how they want their facial hair groomed, and should never trim or alter a mustache or beard without asking first.
Once shaving and facial hair care is complete, clean and dry the supplies, and tidy the area so it is free of any loose hairs. Loose hairs can be irritating in a person’s bed or clothing.
When shaving a person’s body hair, the NA should never assume somebody wants particular hair gone. For example, many women do not shave their legs or underarms by choice. NAs must respect this and take the possibility of these preferences into consideration.
Video by Allie Tiller is licensed under CC BY-NC 4.0
Nail and foot care
Good nail and foot care is essential for a person’s comfort, ease of mobility and the prevention of injury, infection control, and odor prevention. Finger and toenails can collect bacteria under the nails; hangnails, ingrown nails, and torn nails can cause breaks in the skin that provide pathogens a portal of entry. NAs may have to trim and clip a person’s fingernails with a fingernail clipper to keep them smooth and short.
In Illinois, NAs cannot cut or trim a person’s toenails and in other states may not be permitted to trim and clip their fingernails; in situations where NAs cannot trim or clip a nail, the nail should be filed. Clipping finger and toenails can easily cause injuries, and should undertaken with extreme care.
When providing nail care, NAs may have to clean under a person’s hands with an orangewood stick or a similar device. If cleaning under the nails, NAs should soak the nails first, and then gently run the cleaning tool under each nail, rinsing the stick in between cleanings. Nails can be trimmed or filed after they are cleaned.
Foot care for a person with diabetes
People with diabetes will require attentive foot care. Because of their weakened immune system and poor circulation, people with diabetes are highly susceptible to infections of the feet. If their feet are not properly cared for, and if infections are not noticed and addressed early, then the person’s foot may take months to heal and may even need to be amputated. NAs must keep the feet of people with diabetes clean and dry[3].
NAs must examine and clean a diabetic resident’s feet every day with gentle soap. The resident’s feet should be soaked for about 15 – 20 minutes per day and washed with a washcloth. Pat the person’s foot dry when done, and then apply the appropriate lotion. Always check the care plan.
It is important that people with diabetes do not get any cuts or scrapes on their feet. Check the feet thoroughly, including under the toenails, for dry or cracked skin, bumps, temperature changes, and any other abnormalities[4].
Do not trim their toenails; only use a file.
Changing clothes and hospital gowns
Helping someone to change their clothing is a daily task that NAs perform.
One of the most important things to remember when helping a resident dress or undress is to favor their stronger side. Many people will have a side of their body that is weaker than the other, due to aging, stroke, or illness. When dressing a resident, NAs should begin with the weaker side, but when undressing a resident the NA should begin with the stronger side.
Resident must always be allowed to choose their own clothing. NAs can make this process fun by complementing a resident’s sense of style and making them feel fashionable as an enjoyable part of preparing for the day.
Use dressing and undressing time as an opportunity to encourage independence. Dressing and undressing can promote a sense of independence and wellbeing; it is also a great time to work in some range-of-motion exercises. Assistive devices are available for residents who want to dress themselves independently, but have limited range of motion.
4yourCNA. (2016, August 26). Dress a resident with a weak arm CNA skill [Video]. Youtube. https://www.youtube.com/watch?v=PiHCvPHBoZs
If a resident or patient has an IV tube, this may get in the way of undressing and dressing easily. When undressing, the NA should make sure not to remove the IV tube on accident. The IV must remain inserted and cannot be removed for dressing or undressing; the NA will have to take the IV bag from its hook and slip it through the resident’s clothes as they are removed or donned.
When dressing, clothing should be put on the side with the IV tube first; once the clothes on the IV side are one, the NA should hang the IV bag again before proceeding to finish dressing the person. Make sure the IV tube is dripping and is not kinked or obstructed.
Wound Care
Wounds are generally categorized as either open or closed. A closed wound is a wound that does not result in broken skin. Contusions, or bruises, are one form of closed wound. Internal bleeding is another.
When the skin is broken it results in an open wound. Some types of open wounds are abrasions, avulsions, incisions, laceration, and a puncture[5].
- An abrasion is a scrape, and occurs when some of the person’s skin is torn away because of contact with another surface. Abrasions tend to bleed little but still require cleaning and maintenance.
- Avulsion is more serious than an abrasion, and involves a violent tearing of tissue and substantial bleeding.
- Incisions are cuts from sharp objects. Incisions tend to bleed a lot.
- Lacerations are jagged openings caused by tissue being torn apart.
- Puncture wounds are small holes in the skin, caused by pointed objects like a pencil or a nail.
Symptoms of a wound are pain, discoloration, drainage, and observable damage such as bleeding.
The biggest risk to consider when caring for wounds is the possibility of infection, or complications from lack of treatment.
Complications
Wounds negatively impact a person’s basic needs. They cause pain and discomfort, and infected wounds can result in other medical complications including fever and affected appetite. NAs should always allow a person’s pain drugs to take effect before interacting with their wound.
Healing from wounds can be a slow, frustrating, and arduous process. The person may be sad, angry, or hostile. NAs should respond to these behaviors with kindness and compassion, and continue to provide thoughtful care by consistently practicing good communication.
Always meet a frustrated person with care and empathy, especially since the person’s negative feelings are ultimately a result of their pain, not directly in response to the NA.
A person’s belonging and self-esteem needs can also be impacted by wound recovery. Wound recovery, and sometimes life after recovery, will require difficult adjustments, and may produce limitations in a person’s actions, movements, and comfort. NAs should provide a listening ear, and be willing to hear a person’s frustrations with their circumstances in a supportive and professional manner.
Reporting and recording
NAs play an important role in monitoring a wound’s healing process. When observing a wound, NA should take note of its color, size, and shape. Note the type and amount of drainage, and whether the person’s wound dressing needs additional changing.
It is also important to ask the person about their pain levels. After making the observations, NAs should chart them every time, including observations gathered, the, time of observation, and any care given.
Dressing
Wounds must be dressed tightly and securely as an infection control measure. Wound dressings have many important functions, including protecting the wound from further injury or infection, absorbing drainage, removing dead tissues, promoting comfort, covering unsightly wounds, creating an environment conducive to healing, and applying pressure for bleeding control.

Be careful when a person’s wound is dressed with adhesive tape; abrasions can occur when the tape is removed and takes some skin with it. Many people are allergic to adhesive tape.
If tape is used to secure the dressing, it should be placed only at the top, bottom, and middle of the dressing; covering the whole dressing in adhesive tape could obstruct circulation and create discomfort in the event of swelling.
There are many different kinds of wound dressings. The doctor or nurse will determine which kind of dressings to use for a person depending on the type of wound, the wound size and location, drainage, infection, and how frequently the dressing needs to be changed. Always check the care plan.
Skin tears
Skin tears are common wounds in long-term care settings. A skin tear is a break or a rip in the outer layers of skin where the top skin layer separates from the underlying tissues – it can look like the skin is peeled back and the cavity filled with blood. Because older adults tend to have thin and fragile skin, skin tears can be caused by only slight pressure.
The best way NAs can work to prevent skin tears is by consistently providing careful and safe care. Attentively avoiding furniture and corners while ambulating and always making one’s movements gently and smooth are some ways NAs can work to prevent skin tears and further injury. Note a resident’s level of awareness before helping them move or ambulate
Skin tears can be caused by friction, shearing, or pulling and pressure on one’s skin. They can also be caused by falls or bumps on any hard surface. NAs can accidentally cause skin tears by holding on to a person too tightly, removing adhesives, or brushing the resident’s skin against a hard surface while bathing or getting dressed.
Skin tears are infection risks because they are portals of entry for microbes. NA should report skin tears to the nurse at once.
Pressure ulcers
The first thing to keep in mind when learning about how to treat pressure ulcers is that they are much easier to prevent than to cure.
Pressure ulcers occur when a person is in bed for a long period of time and their circulation is reduced; the reduction in circulation can result in the process of skin breakdown or a dying off of skin tissue due to lack of nutrients and oxygen.
Breakdown usually begins in areas with a bony prominence, or an area where the bone sticks out or projects from the flat surface of the body. Some examples are the back of the head, shoulder blades, elbows, hips, spine, knees, ankles, heels, and toes. Bony prominences are also called pressure points.
Risk factors for the formation of pressure ulcers include:
- skin breaks
- poor circulation in a localized area
- excessive moisture or dryness
- irritation caused by waste
- poor nutrition
- dehydration
- wrinkled linens
Pressure ulcers occur when a person is lying or sitting in the same position for too long. This makes people who are comatose, paralyzed, or healing from hip fractures at especially high risk. If a person is at high risk for pressure injuries, and especially if they have altered mental awareness, NAs should take extra care to make sure that person is re-positioned regularly, is free of excess moisture, has healthy skin, and moves to keep their circulation flowing.
The Stages of a Pressure Ulcer: Pressure ulcers progress in 4 stages.
In Stage 1 the ulcer appears red or otherwise discolored, and will be painful and emit a different temperature than the skin around it. It may look like a blister or rash.
In stage 2, the ulcer has shed some layers of skin and will appear red and moist. More layers of skin have corroded.
In stage 3, the ulcer will have shed further layers of skin and may appear yellow, green, brown, or red. The tissues will be sensitive, painful, and moist. Muscle tissue may be visible.
In stage 4, the tissue loss is extensive and may include muscle tissue in addition to lost skin tissue. It will look like a deep pit, and bone may be visible.
Image by Nanoxyde, CC BY-SA 3.0
The areas most at risk for pressure injuries are the side of one’s head, the ear, shoulders, hips, buttocks, knees, ankles, collarbone, under the breasts, on the abdomen, under the scrotum, knees, toes, spinal base or sacrum, between the legs, and on one’s heels. Any place where friction occurs, or where pressure restricts circulation, is a risk factor for pressure ulcers.
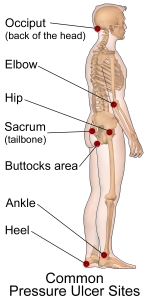
Image by BruceBlaus, CC BY-SA 4.0
The best way to address pressure ulcers is to prevent them before they can form. The nurse will assess a person for their pressure ulcer risk upon admission, and determine what preventative measures to include in their care plan. Managing moisture, good nutrition and fluid balance, and relieving excess pressure are all key measures to preventing pressure ulcers. Always follow the care plan.
Report and record any signs of skin breakdown immediately. NAs should take every opportunity to observe the person’s skin closely, and tell the nurse if any abnormalities are noticed, even if they seem slight or insignificant.
Key Takeaways
- Good hygiene is part of the Big Three, especially Infection Control and Resident Rights. Good hygiene prevents infection and can help residents feel refreshed and ready for the day. Good hygiene is an important part of meeting someone’s basic physical and psychosocial needs.
- Hygiene tasks such as bathing, providing perineal care, and providing oral care will be done daily. Grooming tasks such as nail and hair care will also be done regularly. Always be patient, respectful compassionate, and observant when providing care.
- Observe residents’ skin closely, and report any signs of irritation or breakdown. Skin breakdown in the form of pressure injuries and ulcers is a serious problem, and is easier to prevent than to cure. Providing excellent skin care helps residents feel good, stay clean, and prevents infections.
Comprehension Questions
1) Write a paragraph describing how you would like to be woken up in the morning if you were a resident. What would you like the NA to say to you, and how do you think you’d like to be interacted with? What care tasks would the NA perform as part of morning care?
2) Respond to the following sentences with T (true) or F (false).
____ Partial baths are best for residents who are energetic and mobile.
____ A complete bed bath is for someone who needs a full bath but cannot get out of bed.
____ Residents who are prone to tiredness and become dizzy easily are encouraged to shower.
____ Tub baths are good for people who can transfer into and out of the tub, and who prefer it to using a shower chair.
____ Partial baths include washing the face, underarms, hands, and perineal area.
3) What are some concerns to keep in mind when providing hygiene care? Select any that apply.
- Make sure the water does not exceed 105 degrees.
- Allow residents privacy while bathing by leaving the room. This helps maintain their dignity.
- Promote the person’s independence during personal care by prompting them to do as much of it as they can. Be patient during the process.
- Always follow transmission-based precautions
4) When bathing someone, make sure to dry them thoroughly to …
- Help them stay cool and regulate their temperature
- Prevent bacterial growth in moist areas of the body
- Show them that you are caring for them
- Prevent their linens from becoming damp and causing skin irritation
5) Why is oral care important? Select all that apply.
- Oral care is important for health across the body, and helps prevent gum and heart disease
- It’s a fun experience having one’s teeth brushed
- It helps make a person more confident
- It can make eating a more pleasant experience
6) A resident has developed a thick tangled matte of hair. What should you do?
- Comb it out at all costs – if you pull the tangle out, the discomfort for the resident will be quick.
- Cut it yourself while the resident is sleeping so they don’t have to look at it.
- Discuss it with the resident, and then shave their head.
- Discuss the tangle with the resident and then tell the nurse about it for further planning.
7) Why do the feet of people with diabetes require special attention?
- Their blood sugar builds up in their feet
- They are highly resistant to infection
- Poor circulation and a weakened immune system make them susceptible to infection
- They need soft and thick socks with non-skid soles
8) If a resident has a stroke, then their impacted side will be called the …
- Worse side
- Incapable side
- Weak side
- Impaired side
9) When observing and recording an existing wound, NAs must take note of…
- The wound’s color
- The wound’s size
- The wound’s sound
- The wound’s shape
- The wound’s origin
10) Respond to the following sentences with T (true) or F (false).
____ If a wound’s dressing is damp or loose, it must be changed quickly.
____ Adhesive tape should be removed quickly and forcefully so make it as fast as possible and minimize resident discomfort.
____ NAs should make an informed decision about what dressing to bandage a wound with.
____ Skin tears are caused by lying in the same position for too long and cutting off circulation to a particular area.
____ Frequent repositioning and immediately addressing damp or wrinkled sheets are two ways NAs can help prevent pressure ulcers from forming.
11) Personal care relates closely to the Big Three. Why is providing good personal care such an important part of Resident Rights? Why is it a necessary consideration of Infection Control? What are some Safety considerations NAs must keep in mind while providing personal care, such as while bathing, shaving, and dressing residents?
12) Write a paragraph listing the four stages of pressure ulcers, and describe the characteristics of pressure ulcers at each stage.
- Nursing Assistant (Section 5.6) by Chippewa Valley Technical College is licensed under a Creative Commons Attribution 4.0 International License, ↵
- Dugan, D. (2020). Nursing assisting: A foundation in caregiving (5th ed.), Chapter 12. Hartman. ↵
- Aalaa M, Malazy OT, Sanjari M, Peimani M, Mohajeri-Tehrani M. Nov. 21, 2012. Nurses' role in diabetic foot prevention and care; a review. J Diabetes Metab Disord;11(1):24. doi: 10.1186/2251-6581-11-24 ↵
- Check out this video for more information on providing foot care: https://youtu.be/2v_PMdYPGIs ↵
- Sorrentino, S. A., & Remmert, L. N. (2019). Mosby's essentials for nursing assistants (6th ed.), Chapter 28. Elsevier. ↵
Hygiene, cleanliness, and grooming tasks
Cleaning the genital and anal region
The steps NAs go through every time at the beginning of the care process, including introducing themselves, verifying the resident's identity, and performing hand hygiene.
A small basin that resident’s can use to spit into after rinsing their mouth
The steps followed every time after completing a care task, including performing hand hygiene and making sure the resident is comfortable.
Hair loss
Abnormally high levels of body hair
Excessive shedding of skin flakes
Head lice
Specific container meant for sharp objects like razors and needles and other biohazards
A wound that does not result in open skin, such as a bruise
Wounds with broken skin
A scrape
Tearing of tissue with more substantial bleeding than an abrasion
Cuts made by sharp objects. Surgeons sometimes make incisions; someone may get an incision from a sharp kitchen knife.
Jagged openings from skin being torn apart. An example may be a wound created by scraping against the corner of a piece of furniture.
Small holes in the skin
Skin tears are wounds where the top layer of skin separates from the layers beneath it. It may appear mild at first, but they pose an infection risk.
Corroded skin resulting from persistent pressure in the same place on the body
